General medicine case discussion
Online blended bimonthly assignment toward summative assessment for the month of May 2021
M.SANDHYA
ROLL NO: 89
8th sem
Pulmonology (10 Marks)
A) Link to patient details:
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
3) What could be the causes for her current acute exacerbation?
4. Could the ATT have affected her symptoms? If so how?
5.What could be the causes for her electrolyte imbalance?
1Q) what is the evolution of the symptomatology in this patient interms of an event timeline and where is the anatomical localisation for the problem and what is the primary etiology of the patient problem ?
1Ans)Evolution of symptomatology
1st episode of sob - 20 yr back
2nd episode of sob - 12 yr back
From then she has been having yearly episodes for the past 12 yrs
Diagnosed with diabetis - 8yrs back
Anemia and took iron injections - 5yr ago
Generalised weakness - 1 month back
Diagnosed with hypertension - 20 days back
Pedal edema - 15 days back
Facial puffiness- 15 yrs back
Anatomical location of problem - lungs
Primary etiology of patient- usage of chulha since 20 yrs might be due to chronic usage
2Q)what r the mechanism of action indication and efficacy over placebo of each of the phramacological and nonphramacological interventions used for this patient?
2Ans)~Head end elevation :# MOA;
.improves oxygenation
.decreases incidence VAP
.increases hemodynamic performance
.increases end expiratory lung volume
.decreases incidence of aspiration
#Indication: .head injury
.meningitis
.pneumonia
~ oxygen inhalation to maintain spo2
~Bipap:non invasive method
#MOA :assist ventilation by delivering positive expiratory and inspiratory pressure with out need for ET incubation9
3. Cause for current acute excerbation - it could be due any infection
4.could the ATT affected her symptoms if so how?
Yes ATT affected her symptoms
Isoniazid and rifampcin -nephrotoxic - raised RFT was seen
2) Neurology (10 Marks)
A) Link to patient details:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
3) Why have neurological symptoms appeared this time, that were absent during withdrawal earlier? What could be a possible cause for this?
4) What is the reason for giving thiamine in this patient?
5) What is the probable reason for kidney injury in this patient?
6). What is the probable cause for the normocytic anemia?
7) Could chronic alcoholism have aggravated the foot ulcer formation? If yes, how and why?
I HAVE BEEN GIVEN THE FOLLOWING CASES TO SOLVE IN AN ATTEMPT TO UNDERSTAND THE TOPIC OF PATIENT CLINCAL DATA ANALYSIS TO DEVELOP MY COMPETENCY IN READING AND COMPREHENDING CLINICAL DATA INCLUDING HISTORY,CLINICAL FINDINGS,INVESTIGATIONS AND DIAGNOSIS AND COME UP WITH A TREATMENT PLAN
Add the month of january that year during which time she was working in a paddy field. For the next 8 years the patient has suffered from similar episodes of SOB every year each lasting aproximately 1 week For the past 12 years she has been having an yearly episodes now lasting around a month again around january. Until her latest episode the SOB was of grade II Her latest episode of shortness of breath started 30 days ago, her SOB was insidious in onset and gradual in progression. Initially the SOB occurred on exertion and was relieved upon rest. From 2 days ago she started having SOB even at rest (grade IV) Pedal edema since 15 days upto the level ankle and pitting type OTHER SYMPTOMS Facial puffiness since 15 days. She has drowsiness since 2 days She has decreased urine output for the past 2 days. ANATOMICAL LOCATION; LUNG ALVEOLI PRIMARY ETIOLOGY
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANS
A] Head end elevation
B] O2 inhalation to maintain SPO2 above 92%
C] Intermittent BiPAP for 2hrs
D] Inj. AUGUMENTIN 1.2gm IV BO
MECHANISM OF ACTION;
THIS BLOCKS THE ACTION OF 𝜷 -LACTAMASE
POTASSIUM CLAVULANTA CAN BE INCORPORATED WITH AMOXICILLIN TO FORM AUGUMENTIN
INDICATIONS;
1)lower respiratory tract infection
2)acute bacterial otitis media
3)sinusitis
4)skin and skin structure infections
5)urinary track infections
E] TAB. AZITHROMYCIN 500mg OD
mechanism of action;
Azithromycin binds to the 23S rRNA of the bacterial 50S ribosomal subunit. It stops bacterial protein synthesis by inhibiting the transpeptidation/translocation step of protein synthesis and by inhibiting the assembly of the 50S ribosomal subunit
INDICATIONS;
Azithromycin is an antibiotic. It's widely used to treat chest infections such as pneumonia, infections of the nose and throat such as sinus infection (sinusitis), skin infections, Lyme disease, and some sexually transmitted infections.
F]INJ.LASIX IV BO if SBP GREATER THAN 110 mmHg
mechanism of action;
Furosemide works by blocking the absorption of sodium, chloride, and water from the filtered fluid in the kidney tubules, causing a profound increase in the output of urine (diuresis). The onset of action after oral administration is within one hour, and the diuresis lasts about 6-8 hours
INDICATIONS;Furosemide is a type of medicine called a diuretic. It's used to treat high blood pressure, heart failure and oedema (a build up of fluid in the body). It's also sometimes used to help you pee when your kidneys aren't working properly. Diuretics are sometimes called "water pills/tablets" because they make you pee more.
G] TAB PANTOP 40mg PO OD
The mechanism of action of pantoprazole is to inhibit the final step in gastric acid production. In the gastric parietal cell of the stomach, pantoprazole covalently binds to the H+/K+ ATP pump to inhibit gastric acid and basal acid secretion. The covalent binding prevents acid secretion for up to 24 hours and longer.
INDICATIONS;
It is commonly used for the diagnosis or treatment of Gastro-esophageal reflux disease, Heartburn, Euophagus inflammation, Stomach ulcers. It has some side effects such as Loss of balance, Increased bone fractures, Skin itching, Diarrhea.
H] INJ. HYDROCORTISONE 100 mg
MECHANISM OF ACTION;
Hydrocortisone binds to the glucocorticoid receptor leading to downstream effects such as inhibition of phospholipase A2, NF-kappa B, other inflammatory transcription factors, and the promotion of anti-inflammatory genes
INDICATIONS;
Hydrocortisone is approved by the U.S. Food and Drug Administration as a prescription steroid medication that is indicated to treat inflammation, status asthmaticus, acute and chronic adrenal insufficiency, and as physiologic replacement in pediatric use.
I] IV NEB. with IPRAVENT, BUDECORT 6 hrly
J]TAB PULMOCLEAR 100 mg PO OD
MECHANISM OF ACTION;
They belong to the class of bronchodilators and mucolytics, respectively. Pulmoclear works by relaxing the airways and loosening the cough, thus making the expulsion of cough easy.
INDICATION;
Pulmoclear Tablet is used for relieving the symptoms of coughing, wheezing, congestion and blockage in the airways in a condition called chronic obstructive pulmonary disease (COPD
K] chest physiotherapy
Chest PT, or CPT expands the lungs, strengthens breathing muscles, and loosens and improves drainage of thick lung secretions. Chest PT helps treat such diseases as cystic fibrosis and COPD (chronic obstructive pulmonary disease).
L] GRBS 6 hrly
M] INJ. HAI SC ( 8 am- 2pm- 8pm) Temp, BP, PR, SPO2 monitoring I/O charting
N] INJ. THIAMINE 1 amp in 100 ml of NS )
Mechanism of Action: Thiamine combines with adenosine triphosphate (ATP) in the liver, kidneys, and leukocytes to produce thiamine diphosphate. Thiamine diphosphate acts as a coenzyme in carbohydrate metabolism, in transketolation reactions, and in the utilization of hexose in the hexose-monophosphate shunt.
INDICATIONS;
Thiamine is taken for conditions related to low levels of thiamine, including beriberi and inflammation of the nerves (neuritis) associated with pellagra or pregnancy. Thiamine is also used for digestive problems including poor appetite, ulcerative colitis, and ongoing diarrhea
3. What could be the causes for her current acute exacerbation?
ANS; The most common cause of an exacerbation is infection in the lungs or airways (breathing tubes). This infection is often from a virus, but it may also be caused by bacteria or less common types of organisms
. 4. Could the ATT have affected her symptoms? If so how?
ans; RIFAMPICIN [DAILY OR INTERMITTENT] CAN CAUSES EDEMA BY IMMUNOALLERGIC MECHANISM EDEMA OF LOWER LIMB ARE A POTENTIAL SIGNAL IN PHARMACOVIGILANCE REQUERING MORE INVESTIGATION TO ARGUE WITH THE RELATION OF CAUSE AND EFFECT AND TO FIND RISK FACTOR TO MANAGE AND AVOID THESE EFFECT
5.What could be the causes for her electrolyte imbalance?
ANS; RISK FACTORS
🡻
ACTIVATION OF RAS [RENIN ANGIOTENSIN-ALDOSTERON SYSTEM]
🡻
ELEVATED PLASMA ARGININE VASOPRESSIN
🡻
AGGREVATES ELECTROLYTE IMBALANCE
COMMON FACTORS;
1.RENAL INSUFFICIENCY
2.HYPOXIA
3.HYPERCAPNIA
4.RESPIRATORY ACIDOSIS
5.RIGHT SIDED HEART FAILURE WITH DEVELOPMENT OF
LOWER LIMB EDEMA
6.MALNOURISHED ETC.....
MOST COMMON ELECTROLYTE IS SODIUM ION DECREASES IN COPD
HYPOKALEMIA IS DEU TO TO INDEPENDENTLY OR COMBINED WITH HYPONATREMIA
LOWER LEVEL OF ELECTROLYTE LEADS TO ;
1) DECREASE OF pH
2) DECREASE OF paO2
3) DECREASE OF O2 SATURATION
4) INCREASE OF paCO2
NEUROLOGY
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ans;
evolution of the symptomatology in this patient in terms of an event timeline;
, he had 2-3 episodes of seizures, one being 1 year ago and the most recent being 4 months ago. The most recent time, (4 months ago), he had developed seizures (most probably GTCS) following cessation of alcohol for 24 hours, which was associated with restlessness, sweating, and tremors. Following this episode, he started drinking again.
He was unable to lift himself off the bed and move around, and had to be assisted. It was associated with a decrease in food intake since 9 days
He also had short term memory loss since 9 days
. the primary etiology of the patient's problem
ALOCHOL INTAKE
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ans;
1. IVF NS and RL @150ml/hr
mechanism of action;
Sodium Chloride is source of water and electrolytes. It is capable of inducing diuresis depending on the clinical condition of the patient. It is a crystalloid given intravenously in case of shock, dehydration, and diarrhoea to increase the plasma volume.
indication;
The following are primary indications for the use of normal saline infusion that have been approved by the FDA: Extracellular fluid replacement (e.g., dehydration, hypovolemia, hemorrhage, sepsis) Treatment of metabolic alkalosis in the presence of fluid loss. Mild sodium depletion
2. Inj. 1amp THIAMINE in 100ml NS, TID
Thiamine MOA
Mechanism of Action: Thiamine combines with adenosine triphosphate (ATP) in the liver, kidneys, and leukocytes to produce thiamine diphosphate. Thiamine diphosphate acts as a coenzyme in carbohydrate metabolism, in transketolation reactions, and in the utilization of hexose in the hexose-monophosphate shunt.
Indications and Usage
Thiamine hydrochloride injection should be used where rapid restoration of thiamine is necessary, as in Wernicke's encephalopathy, infantile beriberi with acute collapse, cardiovascular disease due to thiamine deficiency, or neuritis of pregnancy if vomiting is severe.tion;
3. Inj. Lorazepam
mechanism of action;
Lorazepam binds to benzodiazepine receptors on the postsynaptic GABA-A ligand-gated chloride channel neuron at several sites within the central nervous system (CNS). It enhances the inhibitory effects of GABA, which increases the conductance of chloride ions into the cell
indication;
ATIVAN Injection is indicated in adult patients for preanesthetic medication, producing sedation (sleepiness or drowsiness), relief of anxiety, and a decreased ability to recall events related to the day of surgery.
4. T. Pregabalin 75mg/PO/ BD
MECHANISM OF ACTION;
Pregabalin has demonstrated anticonvulsant, analgesic, and anxiolytic properties in preclinical models. The drug's exact mechanism of action is unclear, but it may reduce excitatory neurotransmitter release by binding to the α2-δ protein subunit of voltage-gated calcium channels
INDICATION;
Pregabalin is indicated for the management of neuropathic pain associated with diabetic peripheral neuropathy, postherpetic neuralgia, fibromyalgia, neuropathic pain associated with spinal cord injury, and as adjunctive therapy for the treatment of partial-onset seizures in patients 1 month of age and older
5. Inj. HAI S.C.- premeal
6. GRBS 6th hourly, premeal: 8am, 2pm, 8pm,2am
7. Lactulose 30ml/PO/BD
MECHANISM OF ACTION;
Lactulose is used in preventing and treating clinical portal-systemic encephalopathy. Its chief mechanism of action is by decreasing the intestinal production and absorption of ammonia. It has also gained popularity as a potential therapeutic agent for the management of subacute clinical encephalopathy
INDICATION;Lactulose is a prescription drug used by mouth or rectally to treat or prevent complications of liver disease (hepatic encephalopathy). It does not cure the problem, but may help to improve mental status. Lactulose is a colonic acidifier that works by decreasing the amount of ammonia in the blood.
8. Inj 2 ampoule KCl (40mEq) in 10 NS over 4 hours
MECHANISM OF ACTION;
Potassium ions participate in a number of essential physiological processes, including the maintenance of intracellular tonicity; the transmission of nerve impulses; the contraction of cardiac, skeletal, and smooth muscle; and the maintenance of normal renal function.
INDICATIONS;
Potassium chloride is used to prevent or to treat low blood levels of potassium (hypokalemia). Potassium levels can be low as a result of a disease or from taking certain medicines, or after a prolonged illness with diarrhea or vomiting.
9. Syp Potchlor 10ml in one glass water/PO/BD
Mode of Action ;It helps to maintain potassium balance in the body by restoring normal potassium levels in patients with a low level of potassium...
3) Why have neurological symptoms appeared this time, that were absent during withdrawal earlier? What could be a possible cause for this?
ANS;. Altered sensorium due to alcohol withdrawal syndrome,DECREASE LEVEL OF THIAMINE LEADS TO THE SYMPTOMS
4) What is the reason for giving thiamine in this patient?
ANS;
Thiamine is a key vitamin in the maintenance of membrane integrity and osmotic gradients across cell membranes and is stored in body tissues predominantly as thiamine diphosphate (TDP). TDP participates in energy production as an essential cofactor for several enzymes in the TCA cycle and pentose phosphate pathways
Thiamine deficiency causes depletion of intracellular TDP, leading to a decreased activity of the TCA cycle and pentose phosphate pathways. Consequently, cellular energy (ATP) depletion and reduction of DNA/RNA and NADPH synthesis ensues, which results in low resistance to oxidative stress. Moreover, there is an accumulation of toxic intermediate metabolic products such as lactate, alanine and glutamate, reduced cellular pH in cells, and disruption of the homeostasis of cellular electrolytes, which results in cytotoxic edema.
5) What is the probable reason for kidney injury in this p
6). What is the probable cause for the normocytic anemia?
ANS;
b]neurology
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANS;
the evolution of the symptomatology in this patient in terms of an event timeline
- history of giddiness
This was associated with 1 episode of vomiting on the same day.
from the bed and while walking.
- This was associated with Bilateral Hearing loss, aural fullness and presence of tinnitus.
- He has associated vomiting- 2-3 episodes per day, non projectile, non bilious containing food particles.
- Patient has H/o postural instability- he is unable to walk without presence of supports, swaying is present and he has tendency to fall while walking
PRIMARY ETIOLOGY;
obstruction of the posterior inferior cerebellar artery (PICA, also the most frequent location for a cerebellar infarct) leads to a headache and less commonly vomiting, vertigo, horizontal ipsilateral nystagmus, and truncal ataxia. Anterior inferior cerebellar artery (AICA) territory infarction more often leads to dysmetria, Horner's syndrome, unilateral hearing loss and ipsilateral facial paralysis or anesthesia with contralateral hemibody sensory loss of pain and temperature. Finally, obstruction of the superior cerebellar artery (SCA, located most rostral) tends to produce more ataxia, dysarthria, and nystagmus, with less vertigo, headache, and vomiting. However, presentations can often be atypical or overlap, in particular for hemorrhagic infarcts.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ans;
Tab Veratin 8 mg PO TID
MECHANISM OF ACTION;
Betahistine is one of the few drugs known which is said to improve the microcirculation of the inner ear. It works as a histamine analogue through 2 modes of action(1) agonist of H1 receptors and (2) antagonist of H3 receptors. It has a weak effect on H1 receptors but strong effect on H3 receptors.
INDICATIONS;
Vertin Tablet is used to prevent and treat a disorder of the inner ear known as Ménière's disease. The symptoms include dizziness (vertigo), ringing in the ears (tinnitus), and loss of hearing, probably caused by fluid in the ear.
Inj Zofer 4 mg IV/TID
Mode of Action of Zofer
Zofer Injection works by inhibiting the action of a chemical substance known as serotonin. Serotonin is responsible for inducing nausea and vomiting. Ondansetron binds to a receptor known as 5-HT₃, thus inhibits the binding of serotonin to it and prevents vomiting and nausea.
Tab Ecosprin 75 mg PO/OD
MECHANISM OF ACTION;
Ecosprin is an antiplatelet medicine. It works by inhibiting the action of an enzyme, which makes platelets aggregate together to form a blood clot
INDICATION;
This tablet is also used to prevent heart attacks, stroke and heart-related chest pain (angina)
Tab Atorvostatin 40 mg PO/HS
Mechanism of Action
Atorvastatin competitively inhibits 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase. By preventing the conversion of HMG-CoA to mevalonate, statin medications decrease cholesterol production in the liver
INDICATIONS;
Reduce the risk of non-fatal myocardial infarction.
Reduce the risk of fatal and non-fatal stroke.
Reduce the risk for revascularization procedures.
Reduce the risk of hospitalization for CHF.
Reduce the risk of angina.
BP monitoring- 4rth hourly
Tab Clopidogrel 75 mg PO/OD
MECHANISM OF ACTION;
The active metabolite of clopidogrel selectively inhibits the binding of adenosine diphosphate (ADP) to its platelet P2Y12 receptor and the subsequent ADP- mediated activation of the glycoprotein GPIIb/IIIa complex, thereby inhibiting platelet aggregation. This action is irreversible.
INDICATIONS;
FDA-approved indications for clopidogrel include: Use during a percutaneous coronary intervention (PCI) for acute coronary syndrome (ACS) and stable ischemic heart disease. Primary prevention of thromboembolism atrial fibrillation
Inj Thiamine 1 AMP in 100 ml NSPO/BD
Tab MVT PO/OD
3) Did the patients history of denovo HTN contribute to his current condition?
4) Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic type of stroke?
YES THE PATIENT HAS HISTORY OF CHRONIC ALOCHOLISM AND IS SUSCEPTIBLE TO ISCHEAMIC TYPE OF STROKE
B) Link to patient details:
Questions-
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
3) Did the patients history of denovo HTN contribute to his current condition?
4) Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic type of stroke?
I HAVE BEEN GIVEN THE FOLLOWING CASES TO SOLVE IN AN ATTEMPT TO UNDERSTAND THE TOPIC OF PATIENT CLINCAL DATA ANALYSIS TO DEVELOP MY COMPETENCY IN READING AND COMPREHENDING CLINICAL DATA INCLUDING HISTORY,CLINICAL FINDINGS,INVESTIGATIONS AND DIAGNOSIS AND COME UP WITH A TREATMENT PLAN
Add the month of january that year during which time she was working in a paddy field. For the next 8 years the patient has suffered from similar episodes of SOB every year each lasting aproximately 1 week For the past 12 years she has been having an yearly episodes now lasting around a month again around january. Until her latest episode the SOB was of grade II Her latest episode of shortness of breath started 30 days ago, her SOB was insidious in onset and gradual in progression. Initially the SOB occurred on exertion and was relieved upon rest. From 2 days ago she started having SOB even at rest (grade IV) Pedal edema since 15 days upto the level ankle and pitting type OTHER SYMPTOMS Facial puffiness since 15 days. She has drowsiness since 2 days She has decreased urine output for the past 2 days. ANATOMICAL LOCATION; LUNG ALVEOLI PRIMARY ETIOLOGY
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANS
A] Head end elevation
B] O2 inhalation to maintain SPO2 above 92%
C] Intermittent BiPAP for 2hrs
D] Inj. AUGUMENTIN 1.2gm IV BO
MECHANISM OF ACTION;
THIS BLOCKS THE ACTION OF 𝜷 -LACTAMASE
POTASSIUM CLAVULANTA CAN BE INCORPORATED WITH AMOXICILLIN TO FORM AUGUMENTIN
INDICATIONS;
1)lower respiratory tract infection
2)acute bacterial otitis media
3)sinusitis
4)skin and skin structure infections
5)urinary track infections
E] TAB. AZITHROMYCIN 500mg OD
mechanism of action;
Azithromycin binds to the 23S rRNA of the bacterial 50S ribosomal subunit. It stops bacterial protein synthesis by inhibiting the transpeptidation/translocation step of protein synthesis and by inhibiting the assembly of the 50S ribosomal subunit
INDICATIONS;
Azithromycin is an antibiotic. It's widely used to treat chest infections such as pneumonia, infections of the nose and throat such as sinus infection (sinusitis), skin infections, Lyme disease, and some sexually transmitted infections.
F]INJ.LASIX IV BO if SBP GREATER THAN 110 mmHg
mechanism of action;
Furosemide works by blocking the absorption of sodium, chloride, and water from the filtered fluid in the kidney tubules, causing a profound increase in the output of urine (diuresis). The onset of action after oral administration is within one hour, and the diuresis lasts about 6-8 hours
INDICATIONS;Furosemide is a type of medicine called a diuretic. It's used to treat high blood pressure, heart failure and oedema (a build up of fluid in the body). It's also sometimes used to help you pee when your kidneys aren't working properly. Diuretics are sometimes called "water pills/tablets" because they make you pee more.
G] TAB PANTOP 40mg PO OD
The mechanism of action of pantoprazole is to inhibit the final step in gastric acid production. In the gastric parietal cell of the stomach, pantoprazole covalently binds to the H+/K+ ATP pump to inhibit gastric acid and basal acid secretion. The covalent binding prevents acid secretion for up to 24 hours and longer.
INDICATIONS;
It is commonly used for the diagnosis or treatment of Gastro-esophageal reflux disease, Heartburn, Euophagus inflammation, Stomach ulcers. It has some side effects such as Loss of balance, Increased bone fractures, Skin itching, Diarrhea.
H] INJ. HYDROCORTISONE 100 mg
MECHANISM OF ACTION;
Hydrocortisone binds to the glucocorticoid receptor leading to downstream effects such as inhibition of phospholipase A2, NF-kappa B, other inflammatory transcription factors, and the promotion of anti-inflammatory genes
INDICATIONS;
Hydrocortisone is approved by the U.S. Food and Drug Administration as a prescription steroid medication that is indicated to treat inflammation, status asthmaticus, acute and chronic adrenal insufficiency, and as physiologic replacement in pediatric use.
I] IV NEB. with IPRAVENT, BUDECORT 6 hrly
J]TAB PULMOCLEAR 100 mg PO OD
MECHANISM OF ACTION;
They belong to the class of bronchodilators and mucolytics, respectively. Pulmoclear works by relaxing the airways and loosening the cough, thus making the expulsion of cough easy.
INDICATION;
Pulmoclear Tablet is used for relieving the symptoms of coughing, wheezing, congestion and blockage in the airways in a condition called chronic obstructive pulmonary disease (COPD
K] chest physiotherapy
Chest PT, or CPT expands the lungs, strengthens breathing muscles, and loosens and improves drainage of thick lung secretions. Chest PT helps treat such diseases as cystic fibrosis and COPD (chronic obstructive pulmonary disease).
L] GRBS 6 hrly
M] INJ. HAI SC ( 8 am- 2pm- 8pm) Temp, BP, PR, SPO2 monitoring I/O charting
N] INJ. THIAMINE 1 amp in 100 ml of NS )
Mechanism of Action: Thiamine combines with adenosine triphosphate (ATP) in the liver, kidneys, and leukocytes to produce thiamine diphosphate. Thiamine diphosphate acts as a coenzyme in carbohydrate metabolism, in transketolation reactions, and in the utilization of hexose in the hexose-monophosphate shunt.
INDICATIONS;
Thiamine is taken for conditions related to low levels of thiamine, including beriberi and inflammation of the nerves (neuritis) associated with pellagra or pregnancy. Thiamine is also used for digestive problems including poor appetite, ulcerative colitis, and ongoing diarrhea
3. What could be the causes for her current acute exacerbation?
ANS; The most common cause of an exacerbation is infection in the lungs or airways (breathing tubes). This infection is often from a virus, but it may also be caused by bacteria or less common types of organisms
. 4. Could the ATT have affected her symptoms? If so how?
ans; RIFAMPICIN [DAILY OR INTERMITTENT] CAN CAUSES EDEMA BY IMMUNOALLERGIC MECHANISM EDEMA OF LOWER LIMB ARE A POTENTIAL SIGNAL IN PHARMACOVIGILANCE REQUERING MORE INVESTIGATION TO ARGUE WITH THE RELATION OF CAUSE AND EFFECT AND TO FIND RISK FACTOR TO MANAGE AND AVOID THESE EFFECT
5.What could be the causes for her electrolyte imbalance?
ANS; RISK FACTORS
🡻
ACTIVATION OF RAS [RENIN ANGIOTENSIN-ALDOSTERON SYSTEM]
🡻
ELEVATED PLASMA ARGININE VASOPRESSIN
🡻
AGGREVATES ELECTROLYTE IMBALANCE
COMMON FACTORS;
1.RENAL INSUFFICIENCY
2.HYPOXIA
3.HYPERCAPNIA
4.RESPIRATORY ACIDOSIS
5.RIGHT SIDED HEART FAILURE WITH DEVELOPMENT OF
LOWER LIMB EDEMA
6.MALNOURISHED ETC.....
MOST COMMON ELECTROLYTE IS SODIUM ION DECREASES IN COPD
HYPOKALEMIA IS DEU TO TO INDEPENDENTLY OR COMBINED WITH HYPONATREMIA
LOWER LEVEL OF ELECTROLYTE LEADS TO ;
1) DECREASE OF pH
2) DECREASE OF paO2
3) DECREASE OF O2 SATURATION
4) INCREASE OF paCO2
NEUROLOGY
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ans;
evolution of the symptomatology in this patient in terms of an event timeline;
, he had 2-3 episodes of seizures, one being 1 year ago and the most recent being 4 months ago. The most recent time, (4 months ago), he had developed seizures (most probably GTCS) following cessation of alcohol for 24 hours, which was associated with restlessness, sweating, and tremors. Following this episode, he started drinking again.
He was unable to lift himself off the bed and move around, and had to be assisted. It was associated with a decrease in food intake since 9 days
He also had short term memory loss since 9 days
. the primary etiology of the patient's problem
ALOCHOL INTAKE
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ans;
1. IVF NS and RL @150ml/hr
mechanism of action;
Sodium Chloride is source of water and electrolytes. It is capable of inducing diuresis depending on the clinical condition of the patient. It is a crystalloid given intravenously in case of shock, dehydration, and diarrhoea to increase the plasma volume.
indication;
The following are primary indications for the use of normal saline infusion that have been approved by the FDA: Extracellular fluid replacement (e.g., dehydration, hypovolemia, hemorrhage, sepsis) Treatment of metabolic alkalosis in the presence of fluid loss. Mild sodium depletion
2. Inj. 1amp THIAMINE in 100ml NS, TID
Thiamine MOA
Mechanism of Action: Thiamine combines with adenosine triphosphate (ATP) in the liver, kidneys, and leukocytes to produce thiamine diphosphate. Thiamine diphosphate acts as a coenzyme in carbohydrate metabolism, in transketolation reactions, and in the utilization of hexose in the hexose-monophosphate shunt.
Indications and Usage
Thiamine hydrochloride injection should be used where rapid restoration of thiamine is necessary, as in Wernicke's encephalopathy, infantile beriberi with acute collapse, cardiovascular disease due to thiamine deficiency, or neuritis of pregnancy if vomiting is severe.tion;
3. Inj. Lorazepam
mechanism of action;
Lorazepam binds to benzodiazepine receptors on the postsynaptic GABA-A ligand-gated chloride channel neuron at several sites within the central nervous system (CNS). It enhances the inhibitory effects of GABA, which increases the conductance of chloride ions into the cell
indication;
ATIVAN Injection is indicated in adult patients for preanesthetic medication, producing sedation (sleepiness or drowsiness), relief of anxiety, and a decreased ability to recall events related to the day of surgery.
4. T. Pregabalin 75mg/PO/ BD
MECHANISM OF ACTION;
Pregabalin has demonstrated anticonvulsant, analgesic, and anxiolytic properties in preclinical models. The drug's exact mechanism of action is unclear, but it may reduce excitatory neurotransmitter release by binding to the α2-δ protein subunit of voltage-gated calcium channels
INDICATION;
Pregabalin is indicated for the management of neuropathic pain associated with diabetic peripheral neuropathy, postherpetic neuralgia, fibromyalgia, neuropathic pain associated with spinal cord injury, and as adjunctive therapy for the treatment of partial-onset seizures in patients 1 month of age and older
5. Inj. HAI S.C.- premeal
6. GRBS 6th hourly, premeal: 8am, 2pm, 8pm,2am
7. Lactulose 30ml/PO/BD
MECHANISM OF ACTION;
Lactulose is used in preventing and treating clinical portal-systemic encephalopathy. Its chief mechanism of action is by decreasing the intestinal production and absorption of ammonia. It has also gained popularity as a potential therapeutic agent for the management of subacute clinical encephalopathy
INDICATION;Lactulose is a prescription drug used by mouth or rectally to treat or prevent complications of liver disease (hepatic encephalopathy). It does not cure the problem, but may help to improve mental status. Lactulose is a colonic acidifier that works by decreasing the amount of ammonia in the blood.
8. Inj 2 ampoule KCl (40mEq) in 10 NS over 4 hours
MECHANISM OF ACTION;
Potassium ions participate in a number of essential physiological processes, including the maintenance of intracellular tonicity; the transmission of nerve impulses; the contraction of cardiac, skeletal, and smooth muscle; and the maintenance of normal renal function.
INDICATIONS;
Potassium chloride is used to prevent or to treat low blood levels of potassium (hypokalemia). Potassium levels can be low as a result of a disease or from taking certain medicines, or after a prolonged illness with diarrhea or vomiting.
9. Syp Potchlor 10ml in one glass water/PO/BD
Mode of Action ;It helps to maintain potassium balance in the body by restoring normal potassium levels in patients with a low level of potassium...
3) Why have neurological symptoms appeared this time, that were absent during withdrawal earlier? What could be a possible cause for this?
ANS;. Altered sensorium due to alcohol withdrawal syndrome,DECREASE LEVEL OF THIAMINE LEADS TO THE SYMPTOMS
4) What is the reason for giving thiamine in this patient?
ANS;
Thiamine is a key vitamin in the maintenance of membrane integrity and osmotic gradients across cell membranes and is stored in body tissues predominantly as thiamine diphosphate (TDP). TDP participates in energy production as an essential cofactor for several enzymes in the TCA cycle and pentose phosphate pathways
Thiamine deficiency causes depletion of intracellular TDP, leading to a decreased activity of the TCA cycle and pentose phosphate pathways. Consequently, cellular energy (ATP) depletion and reduction of DNA/RNA and NADPH synthesis ensues, which results in low resistance to oxidative stress. Moreover, there is an accumulation of toxic intermediate metabolic products such as lactate, alanine and glutamate, reduced cellular pH in cells, and disruption of the homeostasis of cellular electrolytes, which results in cytotoxic edema.
5) What is the probable reason for kidney injury in this p
6). What is the probable cause for the normocytic anemia?
ANS;
b]neurology
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANS;
the evolution of the symptomatology in this patient in terms of an event timeline
- history of giddiness
This was associated with 1 episode of vomiting on the same day.
from the bed and while walking.
- This was associated with Bilateral Hearing loss, aural fullness and presence of tinnitus.
- He has associated vomiting- 2-3 episodes per day, non projectile, non bilious containing food particles.
- Patient has H/o postural instability- he is unable to walk without presence of supports, swaying is present and he has tendency to fall while walking
PRIMARY ETIOLOGY;
obstruction of the posterior inferior cerebellar artery (PICA, also the most frequent location for a cerebellar infarct) leads to a headache and less commonly vomiting, vertigo, horizontal ipsilateral nystagmus, and truncal ataxia. Anterior inferior cerebellar artery (AICA) territory infarction more often leads to dysmetria, Horner's syndrome, unilateral hearing loss and ipsilateral facial paralysis or anesthesia with contralateral hemibody sensory loss of pain and temperature. Finally, obstruction of the superior cerebellar artery (SCA, located most rostral) tends to produce more ataxia, dysarthria, and nystagmus, with less vertigo, headache, and vomiting. However, presentations can often be atypical or overlap, in particular for hemorrhagic infarcts.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ans;
Tab Veratin 8 mg PO TID
MECHANISM OF ACTION;
Betahistine is one of the few drugs known which is said to improve the microcirculation of the inner ear. It works as a histamine analogue through 2 modes of action(1) agonist of H1 receptors and (2) antagonist of H3 receptors. It has a weak effect on H1 receptors but strong effect on H3 receptors.
INDICATIONS;
Vertin Tablet is used to prevent and treat a disorder of the inner ear known as Ménière's disease. The symptoms include dizziness (vertigo), ringing in the ears (tinnitus), and loss of hearing, probably caused by fluid in the ear.
Inj Zofer 4 mg IV/TID
Mode of Action of Zofer
Zofer Injection works by inhibiting the action of a chemical substance known as serotonin. Serotonin is responsible for inducing nausea and vomiting. Ondansetron binds to a receptor known as 5-HT₃, thus inhibits the binding of serotonin to it and prevents vomiting and nausea.
Tab Ecosprin 75 mg PO/OD
MECHANISM OF ACTION;
Ecosprin is an antiplatelet medicine. It works by inhibiting the action of an enzyme, which makes platelets aggregate together to form a blood clot
INDICATION;
This tablet is also used to prevent heart attacks, stroke and heart-related chest pain (angina)
Tab Atorvostatin 40 mg PO/HS
Mechanism of Action
Atorvastatin competitively inhibits 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase. By preventing the conversion of HMG-CoA to mevalonate, statin medications decrease cholesterol production in the liver
INDICATIONS;
Reduce the risk of non-fatal myocardial infarction.
Reduce the risk of fatal and non-fatal stroke.
Reduce the risk for revascularization procedures.
Reduce the risk of hospitalization for CHF.
Reduce the risk of angina.
BP monitoring- 4rth hourly
Tab Clopidogrel 75 mg PO/OD
MECHANISM OF ACTION;
The active metabolite of clopidogrel selectively inhibits the binding of adenosine diphosphate (ADP) to its platelet P2Y12 receptor and the subsequent ADP- mediated activation of the glycoprotein GPIIb/IIIa complex, thereby inhibiting platelet aggregation. This action is irreversible.
INDICATIONS;
FDA-approved indications for clopidogrel include: Use during a percutaneous coronary intervention (PCI) for acute coronary syndrome (ACS) and stable ischemic heart disease. Primary prevention of thromboembolism atrial fibrillation
Inj Thiamine 1 AMP in 100 ml NSPO/BD
Tab MVT PO/OD
3) Did the patients history of denovo HTN contribute to his current condition?
4) Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic type of stroke?
YES THE PATIENT HAS HISTORY OF CHRONIC ALOCHOLISM AND IS SUSCEPTIBLE TO ISCHEAMIC TYPE OF STROKE
C) Link to patient details:
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
2) What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
3) What are the changes seen in ECG in case of hypokalemia and associated symptoms?
1Q)What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A) *Evolution of symptoms :patient was normal 8 months back then developed b/l pedal edema which gradually progressed.
Aggerevated in sitting and standing position, relived on taking medication
*Palpitations :since 5days, sudden in onset which is more during night
Aggerevated by lifting heavy weights, speaking continuously
*Dyspnoea during palpitations (NYHA-3) since 5 days
*pain:since 6days, radiating along left upper limb, more during palpitations and relived on medication.
Chest pain associated with chest heaviness since 5 days
Anatomical localisation :
Palpitations
Dyspnoea(NYHA-3)
Pedal edema
Chest pain
Radiating pain along her left upper limb
Etiological agent :
*By localization, electrolyte imbalance (hypokalemia) causing the her manifestations like palpitations, chest heaviness, generalised body weak ness
*radiating pain along her left upper limb due to cervical spondylosis
2Q) What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
A) Reason: recurrent hypokalemic periodic paralysis
Current risk factor:due to use of diuretics
Other risk factors
A) Abnormal loses:
Medications-diuretics, laxatives, enema, corticosteriods
Real causes- osmotic diuresis, mineralo corticoid excess, renal tubular acidosis, hypomagnesenemia
B) trance cellular shift : alkalosis, thyrotoxicosis, delirium tremans, head injury, Myocardial, ischemia, recurrent hypokalemic periodic paralysis
C) Inadequate intake: anorexia, dementia, stareation, total parental nutrition
D) psuedohypokalemia:delayed sample analysis, significant leukocytosis
3) What are the changes seen in ECG in case of hypokalemia and associated symptoms?
A) changes seen in ECG :
Earliest change :decreased T-wave amplitude, ST depression, Twave - and inversion or flat;prolonged PR interval;presence of Uwaves
In Severe cases :ventricular fibrillation, rarely AV block
Symptoms of hypokalemia :
Weakness & fatigue, palpitations, muscle cramps & pain, anxiety, psychosis, depression, delirium.
D) Link to patient details:
QUESTIONS:
1. Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
2. In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
D) Link to patient details:
https://rishikoundinya.blogspot.com/2021/05/55years-old-patient-with-seizures.html
QUESTIONS:
1.Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
seizures after ischaemic strokes. An increase in intracellular Ca2+ and Na+ with a resultant lower threshold for depolarisation, glutamate excitotoxicity, hypoxia, metabolic dysfunction, global hypoperfusion, and hyperperfusion injury
Seizures after haemorrhagic strokes are thought to be attributable to irritation due to (hemosideri. Deposits)caused by products of blood metabolism
Late onset seizures are associated with the persistent changes in neuronal excitability and gliotic scarring is most probably the underlying cause.
2. In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
Initially the patient might have had Simple partial seizures (no loss of consciousness) and might have progressed to Generalised Tonic Clonic seizures (loss of consciousness)
E) Link to patient details:
Questions: 1) What could have been the reason for this patient to develop ataxia in the past 1 year?
2) What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses ?
E) Link to patient details:
https://nikhilasampathkumar.blogspot.com/2021/05/a-48-year-old-male-with-seizures-and.html?m=1
Questions: 1) What could have been the reason for this patient to develop ataxia in the past 1 year?
The patient has minor unattended head injuries in the past 1 yr. Accoding to the CT scan, the patient has cerebral haemorrhage in the frontal lobe causing probably for the occurrence of Frontal love ataxia
2) What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses ?
The patient has minor unattended head injuries. During the course of time the minor hemorrhages if present should have been cured on their own. But the patient is a chronic alcholic. This might have hindered the process of healing or might have stopped the healing rendering it to grow further more into 13 mm sized hemorrhages occupying Frontal Parietal and Temporal lobes
F) Link to patient details:
Questions
1.Does the patient's history of road traffic accident have any role in his present condition?
2.What are warning signs of CVA?
3.What is the drug rationale in CVA?
4. Does alcohol has any role in his attack?
5.Does his lipid profile has any role for his attack??
F) Link to patient details:
http://shivanireddymedicalcasediscussion.blogspot.com/2021/05/a-30-yr-old-male-patient-with-weakness.html
Questions
1.Does the patient's history of road traffic accident have any role in his present condition?
The closeness of facial bones to the cranium would suggest that there are chances of cranial injuries. Since the Zygomatic arch and Mandibular process is very close to the cranium, this might play a role in the patient's present condition
2.What are warning signs of CVA?
Weakness or numbness of the face, arm or leg, usually on one side of the body
Trouble speaking or understanding
Problems with vision, such as dimness or loss of vision in one or both eyes
Dizziness or problems with balance or coordination
Problems with movement or walking
Fainting or seizure
Severe headaches with no known cause, especially if they happen suddenly
3.What is the drug rationale in CVA?
Mannitol- Because of its osmotic effect, mannitol is assumed to decrease cerebral edema. Mannitol might improve cerebral perfusion by decreasing viscosity, and as a free-radical scavenger, it might act as a neuroprotectant.
Ecospirin
For the prevention of heart attack, stroke, heart conditions such as stable or unstable angina (chest pain) due to a blood clot.
Atrovas-Atorva 40 Tablet belongs to a group of medicines called statins. It is used to lower cholesterol and to reduce the risk of heart diseases. Cholesterol is a fatty substance that builds up in your blood vessels and causes narrowing, which may lead to a heart attack or stroke.
Rt feed RT feed is a nursing procedure to provide nutrition to those people who are either unable to obtain nutrition by mouth or are not in a state to swallow the food safely.
4. Does alcohol has any role in his attack?
When the patient met with an accident there might be cranial damage which was unnoticed.
If so his occasional drinking may or may not have hindered the process of the minor hemorrhages getting healed and might have caused this condition
But since the patient is not a chronic alcoholic and so Alcohol might not have played any role.
Therefore it cannot be evaluated without further details
5.Does his lipid profile has any role for his attack??
The inverse relationship between serum HDL-C and stroke risk . When taken together it seems clear that higher baseline levels of serum HDL-C lower the risk of subsequent ischemic stroke.
G) Link to patient details:
__*Questions*_
1)What is myelopathy hand ?
2)What is finger escape ?
3)What is Hoffman’s reflex?
a)what is myelopathy hand?There is loss of power of adduction and extension of the ulnar two or three fingers and an inability to grip and release rapidly with these fingers. These changes have been termed "myelopathy hand" and appear to be due to pyramidal tract involvement.
D
b)what is finger escape?
Finger escape
Wartenberg's sign is a neurological sign consisting of involuntary abduction of the fifth (little) finger, caused by unopposed action of the extensor digiti minimi. . This finding of weak finger adduction in cervical myelopathy is also called the "finger escape sign".
c)what is Hoffman's sign?
Hoffman's sign or reflex is a test used to examine the reflexes of the upper extremities. This test is a quick, equipment-free way to test for the possible existence of spinal cord compression from a lesion on the spinal cord or another underlying nerve condition
H) Link to patient details:
Possible questions:
1) What can be the cause of her condition ?
2) What are the risk factors for cortical vein thrombosis?
3)There was seizure free period in between but again sudden episode of GTCS why?resolved spontaneously why?
4) What drug was used in suspicion of cortical venous sinus thrombosis?
1) What can be the cause of her condition ?
According to MRI cortical vein thrombosis might be the cause of her seizures.
2) What are the risk factors for cortical vein thrombosis?
Infections:
Meningitis, otitis,mastoiditis
Prothrombotic states:
Pregnancy, puerperium,antithrombin deficiency proteinc and protein s deficiency,Hormone replacement therapy.
Mechanical:
Head trauma,lumbar puncture
Inflammatory:
SLE,sarcoidosis,Inflammatory bowel disease.
Malignancy.
Dehydration
Nephrotic syndrome
Drugs:
Oral contraceptives,steroids,Inhibitors of angiogenesis
Chemotherapy:Cyclosporine and l asparginase
Hematological:
Myeloproliferative Malignancies
Primary and secondary polycythemia
Intracranial :
Dural fistula,
venous anomalies
Vasculitis:
Behcets disease wegeners granulomatosis
3)There was seizure free period in between but again sudden episode of GTCS why?resolved spontaneously why?
Seizures are resolved and seizure free period got achieved after medical intervention but sudden episode of seizure was may be due to any persistence of excitable foci by abnormal firing of neurons.
4) What drug was used in suspicion of cortical venous sinus thrombosis?
Anticoagulants are used for the prevention of harmful blood clots.
Clexane ( enoxaparin) low molecular weight heparin binds and potentiates antithrombin three a serine protease Inhibitor to form complex and irreversibly inactivates factor xa.
3) Cardiology (10 Marks)
A) Link to patient details:
1.What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
2.Why haven't we done pericardiocenetis in this pateint?
3.What are the risk factors for development of heart failure in the patient?
4.What could be the cause for hypotension in this patient?
1.What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
Ans:Preserved ejection fraction (HFpEF) – also referred to as diastolic heart failure. The heart muscle contracts normally but the ventricles do not relax as they should during ventricular filling (or when the ventricles relax).
Reduced ejection fraction (HFrEF) – also referred to as systolic heart failure
HFpEF is preceded by chronic comorbidities, such as hypertension, type 2 diabetes mellitus (T2DM), obesity, and renal insufficiency, whereas HFrEF is often preceded by the acute or chronic loss of cardiomyocytes due to ischemia, a genetic mutation, myocarditis, or valvular disease
2.Why haven't we done pericardiocenetis in this pateint?
Ans: Pericardiocentesis is not done here Because the effusion was self healing ,It reduced from 2.4cm to 1.9 cm.
3.What are the risk factors for development of heart failure in the patient?
Ans: risk factors for development of heart faliure in this patent
Alcohol abuse increases the risk of atrial fibrillation, heart attack and congestive heart failure
high blood pressure
Smoking
Diabetes
AV block can be associated with severe bradycardia and hemodynamic instability. It has a greater risk of progressing to third-degree (complete) heart block or asystole.
wosening of pericardial effusion leaing to cardiac tamponade.
4.What could be the cause for hypotension in this
Ans : visceral pericardium may have thickened which is restricting the heart to expand causing hypotension
(May be secondary to TB)
B) Link to patient details:
Questions:
1.What are the possible causes for heart failure in this patient?
2.what is the reason for anaemia in this case?
3.What is the reason for blebs and non healing ulcer in the legs of this patient?
4. What sequence of stages of diabetes has been noted in this patient?
QUESTION: What are the possible causes for heart failure in this patient?
the patient has various comorbidities which could have led to a heart failure
1. The patient was diagnosed with type 2 diabetes mellitus 30 years ago and has been taking human mixtrad insulin daily and was also diagnosed with diabetic triopathy indicating uncontrolled diabetes which is major risk factor for heart failure
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5494155/
2. The patient was also diagnosed with hypertension 19 yrs. ago which is also a risk factor for heart failure
https://pubmed.ncbi.nlm.nih.gov/31472888/
3. He is a chronic alcoholic since 40 years which is a risk factor towards heart failure
https://www.nmcd-journal.com/article/S0939-4753(19)30360-6/fulltext
The findings in this article provide longitudinal evidence that moderate and heavy alcohol consumption are associated with decreased LVEF and trend towards a higher risk of incident LV systolic dysfunction, compared to light drinkers.
4. The patient has elevated creatinine and AST/ALT ratios is >2 and was diagnosed with chronic kidney disease stage IV. CKD is also one of the risk factors for heart failure
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2900793/
QUESTION: what is the reason for anaemia in this case?
The patient has normocytic normochromic anaemia. it could be anaemia of a chronic disease as the patient is diagnosed with CKD stage IV.
Chronic kidney disease results in decreased production of erythropoietin which in turn decreases the production of red blood cells from the bone marrow.
Patient’s with anaemia and CKD also tend to have deficiency in nutrients like iron, vitamin B12 and folic acid essential in making healthy red blood cells
QUESTION: What is the reason for blebs and non-healing ulcer in the legs of this patient?
The most common cause for blebs and non-healing ulcer in this patient is diabetes mellitus. CKD is also known to cause delay in healing of wounds along with poorly controlled diabetes. Anaemia can also slow down the process of healing due to low oxygen levels.
QUESTION: What sequence of stages of diabetes has been noted in this patient?
There are 4 stages in type 2 diabetes- insulin resistance, prediabetes, type 2 diabetes and type 2 diabetes and vascular complications, including retinopathy, nephropathy or neuropathy and, or, related microvascular events.
The patient is diagnosed with diabetic triopathy exhibiting sequence of neuropathy, retinopathy and nephropathy
The patient has been diagnosed with diabetic retinopathy, CKD stage IV and shows signs of diabetic neuropathy such as numbness
C) Link to patient details:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
3) What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
4) What are the risk factors for atherosclerosis in this patient?
5) Why was the patient asked to get those APTT, INR tests for review?
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Ans: *the anatomical site is BLOOD VESSELS;
* ETIOLOGY:
The physical stress of hypertension on the arterial wall also results in the aggravation and acceleration of atherosclerosis, particularly of the coronary and cerebral vessels. Moreover, hypertension appears to increase the susceptibility of the small and large arteries to atherosclerosis.
The most likely cause of arterial thrombosis is artery damage due to atherosclerosis. Atherosclerosis occurs when a person has a buildup of plaque on the walls of their arteries. The arteries then begin to narrow and harden, which increases a person's risk of developing arterial thrombosis.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Ans: PHARMACOLOGICAL INTERVENTIONS
1. TAB. Dytor
mechanism: Through its action in antagonizing the effect of aldosterone, spironolactone inhibits the exchange of sodium for potassium in the distal renal tubule and helps to prevent potassium loss.
2. TAB. Acitrom
mechanism: Acenocoumarol inhibits the action of an enzyme Vitamin K-epoxide reductase which is required for regeneration and maintaining levels of vitamin K required for blood clotting
3. TAB. Cardivas
mechanism:Carvedilol works by blocking the action of certain natural substances in your body, such as epinephrine, on the heart and blood vessels. This effect lowers your heart rate, blood pressure, and strain on your heart. Carvedilol belongs to a class of drugs known as alpha and beta-blockers.
4. INJ. HAI S/C
MECHANISM:Regulates glucose metabolism
Insulin and its analogues lower blood glucose by stimulating peripheral glucose uptake, especially by skeletal muscle and fat, and by inhibiting hepatic glucose production; insulin inhibits lipolysis and proteolysis and enhances protein synthesis; targets include skeletal muscle, liver, and adipose tissue
5.TAB. Digoxin
mechanism:
Digoxin has two principal mechanisms of action which are selectively employed depending on the indication:
Positive Ionotropic: It increases the force of contraction of the heart by reversibly inhibiting the activity of the myocardial Na-K ATPase pump,
an enzyme that controls the movement of ions into the heart.
6. Hypoglycemia symptoms explained
7. Watch for any bleeding manifestations like Petechiae, Bleeding gums.
8. APTT and INR are ordered on a regular basis when a person is taking the anticoagulant drug warfarin to make sure that the drug is producing the desired effect.
3) What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
Ans: *cardiorenal syndrome type 4 is seen in this patient.
4) What are the risk factors for atherosclerosis in this patient?
Ans: effect of hypertention
They can also impair blood vessels' ability to relax and may stimulate the growth of smooth muscle cells inside arteries. All these changes can contribute to the artery-clogging process known as atherosclerosis.
5) Why was the patient asked to get those APTT, INR tests for review?
Ans: APTT and INR are ordered on a regular basis when a person is taking the anticoagulant drug warfarin to make sure that the drug is producing the desired effect.
Here, an INR of 3-4.5 is recommended. Warfarin should be started in conjunction with heparin or low molecular weight heparin when the diagnosis of venous thromboembolism is confirmed, although local protocols may vary in their starting doses and titration schedule.
D) Link to patient details:
Questions-
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
3) What are the indications and contraindications for PCI?
4) What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on overtesting and overtreatment important to current healthcare systems?
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
TIMELINE OF EVENTS-
• Diabetes since 12 years - on medication
• Heart burn like episodes since an year- relieved without medication
• Diagnosed with pulmonary TB 7 months ago- completed full course of treatment, presently sputum negative.
• Hypertension since 6 months - on medication
• Shortness of breath since half an hour-SOB even at rest
Anatomical localisation - Cardiovascular system
Etiology: The patient is both Hypertensive and diabetic , both these conditions can cause
- Atherosclerosis: there is build up of fatty and fibrous material inside the wall of arteries.(PLAQUE)
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Pharmacological interventions:
TAB MET XL 25 MG/STAT-contains Metoprolol as active ingredient
MOA: METOPROLOL is a cardiselective beta blocker
Beta blockers work by blocking the effects of the hormone epinephrine, also known as adrenaline. Beta blockers cause your heart to beat more slowly( negative chronotropic effect)
and with less force( negative inotropic effect). Beta blockers also help open up your veins and arteries to improve blood flow.
Indications: it is used to treat Angina, High blood pressure and to lower the risk of hear attacks .
EFFICACY STUDIES.
Patients were randomized to one of four treatment arms: placebo or ER metoprolol (0.2 mg/kg, 1.0 mg/kg, or 2.0 mg/kg). Data were analyzed on 140 intent-to-treat patients.
Results: mean baseline BP was 132/78 +/- 9/9 mmHg. Following 4 weeks of treatment, mean changes in sitting BP were: placebo = -1.9/-2.1 mmHg; ER metoprolol 0.2 mg/kg = -5.2/-3.1 mmHg; 1.0 mg/kg = -7.7/-4.9 mmHg; 2.0 mg/kg = -6.3/-7.5 mmHg. Compared with placebo, ER metoprolol significantly reduced systolic blood pressure (SBP) at the 1.0 and 2.0 mg/kg dose (P = .027 and P = .049, respectively), reduced diastolic blood pressure (DBP) at the 2.0 mg/kg dose (P = .017), and showed a statistically significant dose response relationship for the placebo-corrected change in DBP from baseline. There were no serious adverse events or adverse events requiring study drug discontinuation among patients receiving active therapy.
Non pharmacological intervention advised to this patient is: PERCUTANEOUS CORONARY INTERVENTION.
Percutaneous Coronary Intervention is a non-surgical procedure that uses a catheter (a thin flexible tube) to place a small structure called a stent to open up blood vessels in the heart that have been narrowed by plaque buildup ( atherosclerosis).
3) What are the indications and contraindications for PCI?
INDICATIONS:
Acute ST-elevation myocardial infarction (STEMI)
Non–ST-elevation acute coronary syndrome (NSTE-ACS)
Unstable angina.
Stable angina.
Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)
High risk stress test findings.
CONTRAINDICATIONS:
Intolerance for oral antiplatelets long-term.
Absence of cardiac surgery backup.
Hypercoagulable state.
High-grade chronic kidney disease.
Chronic total occlusion of SVG.
An artery with a diameter of <1.5 mm.
4) What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on overtesting and overtreatment important to current healthcare systems?
Although PCI is generally a safe procedure , it might cause serious certain complications like
A)Bleeding
B) Blood vessel damage
C) Allergic reaction to the contrast dye used
D) Arrhythmias
E) Need for emergency coronary artery bypass grafting .
Because of all these complications it is better to avoid PCI in patients who do not require it.
⁃ OVER TESTING AND OVER TRAETMENT HAVE BECOME COMMMIN IN TODAY’S MEDICAL PRACTICE.
⁃ Research on overtesting and overtreatment is important as they are more harmful than useful.
Harms to patients
. Performing screening tests in patients with who at low risk for the disease which is being screened.
For example:Breast Cancer Screenings Can Cause More Harm Than Good in Women Who Are at Low Risk. A harmless lump or bump could incorrectly come up as cancer during routine breast screenings. This means that some women undergo surgery, chemotherapy or radiation for cancer that was never there in the first place.
.Overuse of imaging techniques such as X- RAYS AND CT SCANS as a part of routine investigations.
Overuse of imaging can lead to a diagnosis of a condition that would have otherwise remained irrelevant - OVERDIAGNOSIS.
Also the adverse effects due to this are more when compared to the benefits.
.Overdiagnosis through overtesting can psychologically harm the patient.
Hospitalizations[41] for those with chronic conditions who could be treated as outpatients[ can lead to economic burden and a feeling of isolation.
Harms to health care systems
The use of expensive technologies and machineries are causing burden on health care systems.
E) Link to patient details:
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
3) Did the secondary PTCA do any good to the patient or was it unnecessary?
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Ans: *the anatomical location ofetiology is BLOOD VESSELS.
*myocardial infarction is usually due to thrombotic occlusion of a coronary vessel caused by rupture of a vulnerable plaque. Ischemia induces profound metabolic and ionic perturbations in the affected myocardium and causes rapid depression of systolic function
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Ans: PHARMACOLOGICAL INNTERVENTION
1.TAB. ASPIRIN
mechanism:Aspirin inhibits platelet function through irreversible inhibition of cyclooxygenase (COX) activity. Until recently, aspirin has been mainly used for primary and secondary prevention of arterial antithrombotic events.
2.TAB ATORVAS
mechanism:Atorvastatin competitively inhibits 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase. By preventing the conversion of HMG-CoA to mevalonate, statin medications decrease cholesterol production in the liver.
3.TAB CLOPIBB
mechanism:The active metabolite of clopidogrel selectively inhibits the binding of adenosine diphosphate (ADP) to its platelet P2Y12 receptor and the subsequent ADP- mediated activation of the glycoprotein GPIIb/IIIa complex, thereby inhibiting platelet aggregation. This action is irreversible.
4.INJ HAI
mechanism:Regulates glucose metabolism
Insulin and its analogues lower blood glucose by stimulating peripheral glucose uptake, especially by skeletal muscle and fat, and by inhibiting hepatic glucose production; insulin inhibits lipolysis and proteolysis and enhances protein synthesis; targets include skeletal muscle, liver, and adipose tissue
5.ANGIOPLASTY
mechanism:Angioplasty, also known as balloon angioplasty and percutaneous transluminal angioplasty (PTA), is a minimally invasive endovascular procedure used to widen narrowed or obstructed arteries or veins, typically to treat arterial atherosclerosis.
3) Did the secondary PTCA do any good to the patient or was it unnecessary?
Ans:the second PCI was NOT necessary in this patient.
PCI performed from 3 to 28 days after MI does not decrease the incidence of death, reinfarction or New York Heart Association (NYHA) class IV heart failure but it is associated with higher rates of both procedure-related and true ST elevation reinfarction.3 A retrospective analysis of the clinical data revealed The Thrombolysis in Myocardial Infarction (TIMI) Risk Score of 4 predicting a 30-day mortality of 7.3% in this patient. Late PCI leads to the increased risks of periprocedural complications, long-term bleeding, and stent thrombosis.
The high incidence of CAD and the increasing need for PCI provides an opportunity to evaluate its appropriate use and highlight potential overuse. PCI is frequently reported to be overused and inappropriately recommended. Behnke et al defined overuse as ‘use of unnecessary care when alternatives may produce similar outcomes, resulting in a higher cost without increased value’.8Overuse causes a heavy financial burden on people living in countries, where fee-for-service and ill-regulated private healthcare provides much of the patient care. As a result, cost of healthcare increases and causes potential harm to the patients.
F) Link to patient details:
1. How did the patient get relieved from his shortness of breath after i.v fluids administration by rural medical practitioner?
2. What is the rationale of using torsemide in this patient?
3. Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
1. How did the patient get relieved from his shortness of breath after i.v fluids administration by rural medical practitioner?
Because of the fluid loss occurred to the patient
there is decreased preload- so, SOB occurred due to decreased CO
IV fluids administered- there is increased preload- SOB decreased due to better of cardiac output.
2. What is the rationale of using torsemide in this patient?
Torsemide used to relieve abdominal distension.
3. Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
IT IS THE TREATMENT FOR UTI
Rationale- Used for any bacterial infection.
A) Link to patient details:
QUESTIONS:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
Gastroenterology (& Pulmonology) 10 Marks
A) Link to patient details:
https://63konakanchihyndavi.blogspot.com/2021/05/case-discussion-on-pancreatitis-with.html
QUESTIONS:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Evolution of symptomatology
H5 years back-1st episode of pain abdomen and vomitings
Stopped taking alcohol for 3 years
1 year back 5 to 6 episodes of pain abdomen and vomitings after starting to drink alcohol again
20 days back increased consumption of toddy intake
Since 1 week pain abdomen and vomiting
Since 4 days fever constipation and burning micturition
Anatomical localisation: Pancreas and left lung
Alcohol and its metabolites produce changes in the acinar cells, which may promote premature intracellular digestive enzyme activation thereby predisposing the gland to autodigestive injury. Pancreatic stellate cells (PSCs) are activated directly by alcohol and its metabolites and also by cytokines and growth factors released during alcohol-induced pancreatic necroinflammation. Activated PSCs are the key cells responsible for producing the fibrosis of alcoholic chronic pancreatitis
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
A) * Non pharmacological interventions : drains ( malecot & icd )
* Even i as a treating physician will follow the same approach
B) Link to patient details:
1) What is causing the patient's dyspnea? How is it related to pancreatitis?
2) Name possible reasons why the patient has developed a state of hyperglycemia.
3) What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
4) What is the line of treatment in this patient?
the cause of dyspnea might be PLEURAL EFFUSION
b)
*This hyperglycemia could thus be the result of a hyperglucagonemia secondary to stress
* the result of decreased synthesis and release of insulin secondary to the damage of pancreatic β-cells
* elevated levels of catecholamines and cortisol
c)
LFT are increased due to hepatocyte injury
*If the liver is damaged or not functioning properly, ALT can be released into the blood. This causes ALT levels to increase. A higher than normal result on this test can be a sign of liver damage.
*elevated alanine transaminase (ALT) and aspartate transaminase (AST), usually one to four times the upper limits of normal in alcoholic fatty liver.
The reasons for a classical 2:1 excess of serum AST activity compared to serum ALT activity in alcoholic hepatitis have been attributed to
(i) decreased ALT activity most likely due to B6 depletion in the livers of alcoholics
(ii) mitochondrial damage leading to increased release of mAST in serum.
d)
Plan of action and Treatment:
Investigations:
✓ 24 hour urinary protein
✓ Fasting and Post prandial Blood glucose
✓ HbA1c
✓ USG guided pleural tapping
Treatment:
• IVF: 125 mL/hr
• Inj PAN 40mg i.v OD
• Inj ZOFER 4mg i.v sos
• Inj Tramadol 1 amp in 100 mL NS, i.v sos
• Tab Dolo 650mg sos
• GRBS charting 6th hourly
• BP charting 8th hourly
C) Link to patient details:
Possible Questions :-
1) what is the most probable diagnosis in this patient?
2) What was the cause of her death?
3) Does her NSAID abuse have something to do with her condition? How?
1) What is the most probable diagnosis in this patient?
àDifferential Diagnosis:
· Ruptured Liver Abscess.
· Organized collection secondary to Hollow viscous Perforation.
· Organized Intraperitoneal Hematoma.
· Free fluid with internal echoes in Bilateral in the Subdiaphragmatic space.
· Grade 3 RPD of right Kidney
àThe most probably diagnosis is there is abdominal hemorrhage. This will give reasoning to the abdominal distention, and the blood which is aspirated.

2) What was the cause of her death?
àAfter leaving the hospital, the patient went to Hyderabad and underwent an emergency laparotomy surgery. The patient passed away the next day. Cause of her death can be due to complications of laparotomy surgery such as, hemorrhage (bleeding), infection, or damage to internal organs.

3) Does her NSAID abuse have something to do with her condition? How?
àNSAID-induced renal dysfunction has a wide spectrum of negative effects, including decreased glomerular perfusion, decreased glomerular filtration rate, and acute renal failure. Chronic NSAIDs use has also been related to hepatotoxicity. While the major adverse effects of NSAIDs such as gastrointestinal mucosa injury are well known, NSAIDs have also been associated with hepatic side effects ranging from asymptomatic elevations in serum aminotransferase levels and hepatitis with jaundice to fulminant liver failure and death
5) Nephrology (and Urology) 10 Marks
A) Link to patient details:
1. What could be the reason for his SOB ?
2. Why does he have intermittent episodes of drowsiness ?
3. Why did he complaint of fleshy mass like passage in his urine?
4. What are the complications of TURP that he may have had?
Liver abscess
1ans- yes, it could be due to intake of contaminated toddy
2ans - according to some studies, alcoholism mainly consuming locally prepared alcohol plays a major role as a predisposing factor for the formation of liver abscesses that is both amoebic as well as pyogenic liver abscess because of the adverse effects of alcohol over the Liver.
3ans-yes right lobe is involved due to its moreblood supply
4ans- Indications for USG guided aspiration of liver abscess
1. Large abscess more than 6cms
2. Left lobe abscess
3.Caudate lobe abscess
4. Abscess which is not responding to drugs
B) Link to patient details:
Questions
1.Why is the child excessively hyperactive without much of social etiquettes ?
2. Why doesn't the child have the excessive urge of urination at night time ?
3. How would you want to manage the patient to relieve him of his symptoms?
Link to patient details:
https://drsaranyaroshni.blogspot.com/2021/05/an-eight-year-old-with-frequent.html
Questions
1.Why is the child excessively hyperactive without much of social etiquettes ?
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder characterized by inattention, or excessive activity and impulsivity, which are otherwise not appropriate for a person's age
For a diagnosis, the symptoms have to be present for more than six months, and cause problems in at least two settings (such as school, home, work, or recreational activities).
2. Why doesn't the child have the excessive urge of urination at night time ?
Since the child doesn’t have excessive urge of urination at night but at day there might be a psychiatry related condition
1. Psychosomatic disorder
2. Undiagnosed anxiety disorder
3. How would you want to manage the patient to relieve him of his symptoms?
bacterial kidney infection, the typical course of treatment is antibiotic and painkiller therapy.
If the cause is an overactive bladder, a medication known as an anticholinergic may be used. These prevent abnormal involuntary detrusor muscle contractions from occurring in the wall of the bladder
To treat attention deficit hyperactivity disorder:
For children 6 years of age and older, the recommendations include medication and behavior therapy together — parent training in behavior management for children up to age 12 and other types of behavior therapy and training for adolescents. Schools can be part of the treatment as well.
Methylphenidate A stimulant and a medication used to treat Attention Deficit Hyperactivity Disorder. It can make you feel very ‘up’, awake, excited, alert and energised, but they can also make you feel agitated and aggressive. They may also stop you from feeling hungry.
Amphetamine belongs to a class of drugs known as stimulants. It can help increase your ability to pay attention, stay focused on an activity, and control behavior problems. It may also help you to organize your tasks and improve listening skills.
6) Infectious Disease (HI virus, Mycobacteria, Gastroenterology, Pulmonology) 10 Marks
A) Link to patient details:
Questions:
1.Which clinical history and physical findings are characteristic of tracheo esophageal fistula?
2) What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
QUESTION 1:
1.Which clinical history and physical findings are characteristic of tracheo esophageal fistula?
ANSWER:
Cough since 2 months on taking food and liquids
•difficulty in swallowing since 2 month . It was initially difficult only with solids but then followed by liquids also.
•laryngeal crepitus- positive
These favour for tracheo esophageal.fistula
QUESTION 2:
2) What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
ANSWER:
Immune reconstitution inflammatory syndrome (IRIS) represents the worsening of a recognized (paradoxical IRIS) or unrecognized (unmasking IRIS) pre-existing infection in the setting of improved immunologic function.
The most effective prevention of IRIS would involve initiation of ART before the development of advanced immunosuppression. IRIS is uncommon in individuals who initiate antiretroviral treatment with a CD4+ T-cell count greater than 100 cells/uL.
Aggressive efforts should be made to detect asymptomatic mycobacterial or cryptococcal disease prior to the initiation of ART, especially in areas endemic for these pathogens and with CD4 T-cell counts less than 100 cells/uL.
Two prospective randomized studies are evaluating prednisone and meloxicam for the prevention of paradoxical TB IRIS.
7) Infectious disease and Hepatology:
Link to patient details:
1. Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors
present in it ?
What could be the cause in this patient ?
2. What is the etiopathogenesis of liver abscess in a chronic alcoholic patient ? ( since 30 years - 1 bottle per day)
3. Is liver abscess more common in right lobe ?
4.What are the indications for ultrasound guided aspiration of liver abscess ?
Liver abscess
1Q)do u think drinking locally made alcohol cause liver abscess in this patient due to predisposing factors present in it ? What could be the cause in this patient?
1ans- yes, it could be due to intake of contaminated toddy
2Q)what is the etiopathogenesis of liver abscess in a chronic alcoholic patient?(since 30 yrs - 1 bottle/day)
2ans - according to some studies, alcoholism mainly consuming locally prepared alcohol plays a major role as a predisposing factor for the formation of liver abscesses that is both amoebic as well as pyogenic liver abscess because of the adverse effects of alcohol over the Liver. It is also proven that Alcoholism is never an etiological factor for the formation of liver abscess.
3Q)is liver abscess is more common in right lobe?
3ans-yes right lobe is involved due to its moreblood supply
4Q) what r the indications for usg guided aspiration of liver abscess
4ans- Indications for USG guided aspiration of liver abscess
1. Large abscess more than 6cms
2. Left lobe abscess
3.Caudate lobe abscess
4. Abscess which is not responding to drugs
B) Link to patient details:
QUESTIONS:
1) Cause of liver abcess in this patient ?
2) How do you approach this patient ?
3) Why do we treat here ; both amoebic and pyogenic liver abcess?
4) Is there a way to confirmthe definitive diagnosis in this patient?
1) Cause of liver abcess in this patient ?
1ans:cause of liver abcess in this patient is ENTAMOEBA HISTOLYTICA

2) How do you approach this patient ?
2 ans:APPROACH IN THE PATIENT OF AMOEBIC LIVER ABCESS

3) Why do we treat here ; both amoebic and pyogenic liver abcess
3ans:we treat the paient for both amoebic and pyogenic abcess so that we dont rely only on anti-amebic therapy and insure comple treatment of the cause
4) Is there a way to confirmthe definitive diagnosis in this patient?
4 ans: he confirmatory test for amoebic abcess is
*Serologic testing is the most widely used method of diagnosis for amebic liver abscess. In general, the test result should be positive, even in cases when the result of the stool test is negative (only extraintestinal disease).
*The diagnosis of amebic liver abscess was based on four or more of the following criteria:
(i) a space-occupying lesion in the liver diagnosed by ultrasonography and suggestive of abscess,
(ii) clinical symptoms (fever, pain in the right hypochondrium (often referred to the epigastrium), lower chest, back, or tip of the right shoulder),
(iii) enlarged and/or tender liver, usually without jaundice,
(iv) raised right dome of the diaphragm on chest radiograph, and
(v) improvement after treatment with antiamebic drugs (e.g., metronidazole).
8) Infectious disease (Mucormycosis, Ophthalmology, Otorhinolaryngology, Neurology) 10 Marks
A) Link to patient details:
Questions :
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
3) What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
QUESTION: What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary aetiology of the patient's problem?
1. 3 years ago- diagnosed with hypertension
2. 21 days ago- received vaccination at local PHC which was followed by fever associated with chills and rigors, high grade fever, no diurnal variation which was relieved on medication
3. 18 days ago- complained of similar events and went to the the local hospital, it was not subsided upon taking medication(antipyretics)
4. 11 days ago - c/o Generalized weakness and facial puffiness and periorbital oedema. Patient was in a drowsy state
5. 4 days ago-
a. patient presented to casualty in altered state with facial puffiness and periorbital oedema and weakness of right upper limb and lower limb
b. towards the evening patient periorbital oedema progressed
c. serous discharge from the left eye that was blood tinged
d. was diagnosed with diabetes mellitus
6. patient was referred to a government general hospital
7. patient died 2 days ago
patient was diagnosed with diabetic ketoacidosis and was unaware that he was diabetic until then. This resulted in poorly controlled blood sugar levels. The patient was diagnosed with acute oro rhino orbital mucormycosis . rhino cerebral mucormycosis is the most common form of this fungus that occurs in people with uncontrolled diabetes ( https://www.cdc.gov/fungal/diseases/mucormycosis/definition.html ) the fungus enters the sinuses from the environment and then the brain.
The patient was also diagnosed with acute infarct in the left frontal and temporal lobe. Mucormycosis is associated with the occurrence of CVA ( https://journal.chestnet.org/article/S0012-3692(19)33482-8/fulltext#:~:text=There%20are%20few%20incidences%20reported,to%20better%20morbidity%2Fmortality%20outcomes. )
QUESTION: What is the efficacy of drugs used along with other non-pharmacological treatment modalities and how would you approach this patient as a treating physician?
The proposed management of the patient was –
1. inj. Liposomal amphotericin B according to creatinine clearance
2. 200mg Iitraconazole was given as it was the only available drug which was adjusted to his creatinine clearance
3. Deoxycholate was the required drug which was unavailable
https://pubmed.ncbi.nlm.nih.gov/23729001/ this article talks about the efficacy and toxicity of different formulations of amphotericin B
along with the above mentioned treatment for the patient managing others symptoms is also done by-
I. Management of diabetic ketoacidosis –
(a) Fluid replacement- The fluids will replace those lost through excessive urination, as well as help dilute the excess sugar in blood.
(b) Electrolyte replacement-The absence of insulin can lower the level of several electrolytes in blood. Patient will receive electrolytes through a vein to help keep the heart, muscles and nerve cells functioning normally.
(c) Insulin therapy- Insulin reverses the processes that cause diabetic ketoacidosis. In addition to fluids and electrolytes, patient will receive insulin therapy
QUESTION: What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
Mucormycosis is may be being triggered by the use of steroids, a life-saving treatment for severe and critically ill Covid-19 patients. Steroids reduce inflammation in the lungs for Covid-19 and appear to help stop some of the damage that can happen when the body's immune system goes into overdrive to fight off coronavirus. But they also reduce immunity and push up blood sugar levels in both diabetics and non-diabetic Covid-19 patients.
With the COVID-19 cases rising in India the rate of occurrence of mucormycosis in these patients is increasing
9) Infectious Disease (Covid 19)
As these patients are currently taking up more than 50% of our time we decided to make a separate log link here:
for this question that contains details of many of our covid 19 patients documented over this month and we would like you to:
1) Sort out these detailed patient case report logs into a single web page as a master chart
2) In the master chart classify the patient case report logs into mild, moderate severe and
3) indicate for each patient, the day of covid when their severity changed from moderate to severe or vice versa recognized primarily through increasing or decreasing oxygen requirements
4) Indicate the sequence of specific terminal events for those who died with severe covid (for example, altered sensorium, hypotension etc).
9) Infectious Disease (Covid 19)
As these patients are currently taking up more than 50% of our time we decided to make a separate log link here:
http://medicinedepartment.blogspot.com/2021/05/covid-case-report-logs-from-may-2021.html?m=1
for this question that contains details of many of our covid 19 patients documented over this month and we would like you to:
1) Sort out these detailed patient case report logs into a single web page as a master chart
2) In the master chart classify the patient case report logs into mild, moderate severe and
3) indicate for each patient, the day of covid when their severity changed from moderate to severe or vice versa recognized primarily through increasing or decreasing oxygen requirements
4) Indicate the sequence of specific terminal events for those who died with severe covid (for example, altered sensorium, hypotension etc).
https://docs.google.com/spreadsheets/d/e/2PACX-1vQuWFPoQm48IiBs1aDOGHPMosE9sylv2WdixecZa7xbmudlxrGMxk1O_1fgKpNxBbNPZLpIy37oQPcy/pubhtml
1) Covid 19 with co morbidity (Pulmonology/Rheumatology)
https://nikhilasampathkumar.blogspot.com/2021/05/covid-pneumonia-in-pre-existing-case-of.html
Questions:
1) How does the pre-existing ILD determine the prognosis of this patient?
The pre-existing ILD significantly worsens the prognosis of this covid patient.
Interstitial lung disease is characterized by dyspnea, decreased pulmonary diffusing capacity, decreased FVC and TLC. The SpO2 of these patients is usually decreased due to increased A-a gradient
A superimposed covid-19 infection in these cases can cause an acute exacerbation of symptoms such as dyspnea, decreasing levels of SpO2 further and faster than in Covid-19 patients without interstitial lung disease.
Radiology (HRCT) usually shows the development of new pulmonary opacities and fibrosis.
Patient factors:
Since this patient already had a reduced SpO2 of 90-92% (compared to the normal range of >96%) she is more susceptible to worsening of hypoxia and dyspnea unless immediate ventilator support is provided
The patient reportedly did not have dyspnea prior to the covid infection but developed a grade 2 SOB
ILD by itself makes the patient much more susceptible to acquiring Covid-19 infection.
Prognosis: Poor
Source: https://ejrnm.springeropen.com/articles/10.1186/s43055-021-00431-2
2) Why was she prescribed clexane (enoxaparin)?
The main pathogenesis of systemic inflammation caused by Covid-19 is by inducing a cytokine storm that causes epithelial cell necrosis, increased vascular permeability, dysfunctional humoral and CMI which all collectively lead to acute lung injury and ARDS
Of these cytokines, IL-6 is one that is the most important in determining the prognosis. IL-6 levels are highly elevated in patients with severe disease
Enoxaparin is said to relieve and prevent inflammation produced by IL-6 by inactivating it by binding it with its non-anticoagulant fraction, especially in pulmonary epithelial cells.
Moreover, patients with Covid-19 are more susceptible to the development of venous thromboembolism, which can be prevented by Enoxaparin (LMWH).
CASE 9-2: COVID-19 SEVERE
https://nehapradeep99.blogspot.com/2021/05/a-50-year-old-female-with-viral.html
QUESTIONS:
1) Since patient didn't show any previous characteristic diabetes signs, did the Covid-19 infection aggravate any underlying condition and cause the indolent diabetes to express itself? If so what could be the biochemical pathways that make it plausible?
The patient may have already had slight hyperglycemia, owing to high HbA1c levels (7.1%), which may have aggravated due to COVID-19. The possible biochemical pathways include: [6]
2) Did the patient's diabetic condition influence the progression of her pneumonia?
Yes, with DM or hypergycemia in patients leads to an increase in COVID-19 severity. Also, poor glycaemic control predicts an increased need for medications and hospitalizations, and increased mortality.
In monocytes: elevated glucose levels increase SARS-CoV-2 replication, and glycolysis sustains SARS-CoV-2 replication via the production of mitochondrial reactive oxygen species and activation of hypoxia-inducible factor 1α. Therefore, hyperglycaemia supports viral proliferation.
3) What is the role of D Dimer in the monitoring of covid? Does it change management or would be considered overtesting?
D- Dimer levels indicate the severity of COVID-19, pertaining to possible thrombotic complications- as D Dimer is formed post- fibrinolysis.
D- Dimer does change the management, as D-Dimer levels above 2000ng/dl were found to have a direct link with increasing severity of COVID-19 [7]. Moreover, D- dimer levels would be helpful in fast diagnosis and prevention of thrombotic complications.
CASE 9-3 (COVID-19 SEVERE)
https://143vibhahegde.blogspot.com/2021/05/covid-in-26-yo-female.html
QUESTIONS:
1. Why was this patient given noradrenaline?
Following kidney failure, the patient had sudden and persistent hypotension. To combat this, the patient was given noradrenaline, a potent vasoconstrictor.
2. What is the reason behind testing for LDH levels in this patient?
LDH (Lactate Dehydrogenase) catalyzes the conversion of lactate to pyruvate and back. Hence, an increase in LDH denotes some form of tissue damage. In this patient, an increase in LDH levels would denote inflammation, and a high increase would denote Multi-Organ Failure.
3. What is the reason for switching from BiPAP to mechanical ventilation with intubation in this patient? What advantages did it provide?
Although BiPaP is a positive pressure system, unlike tracheal intubation, it does not send the air to the trachea and depends on the patient's ability to respire. In this patient, as SpO2 levels were dropping to 30% despite BiPAP, a more invasive method was required to push the air directly into the lungs- hence intubation was preferred.
CASE 9-4 (COVID-19 MILD)
https://gsuhithagnaneswar.blogspot.com/2021/05/29-year-old-male-patient-with-viral.html?m=1
QUESTIONS:
1. Is the elevated esr due to covid related inflammation?
Yes, as ESR is an important indicator of immunological loss, and owing to an increased inflammation and immunological dysfunction in COVID, elevated ESR is most likely dur to COVID related inflammation.
2. What was the reason for this patient's admission with mild covid? What are the challenges in home isolation and harms of hospitalization?
Hospitalisation was due to Grade 3 Shortness of Breath (SOB), and long duration of COVID-19 infection.
Challenges of home isolation-
Physical challenges- Many patients may find it hard to cut themselves from the outside world and confine themselves to a room for long periods of time
Emotional challenges- Sitting in a small room all day leads to stress, anxiety and even depression, with an increase in mental health issues being reported during the pandemic
Social challenges- Members of society who cannot care for themselves on their own (eg, patients with disability, geriatric patients etc) are at a major loss
Economic challenges- Some patients, such as daily wage labourers, cannot afford to home isolate as they need to earn on a daily basis to keep their family going
Harms of hospitalisation-
Infection- Members visiting may get COVID from exposure to the hospital ward alone
Cost- PAtient may not be able to bear the brunt of high costs
Overtesting- Hospitals may ask the patients to stay overnight despite the conditions being mild, based on preliminary test results
Economic- Working patients may have to take a leave of absence, hence affecting both their work and decreasing their salary, on top of spending money on hospitalisation
CASE 9-5 (COVID-19 SEVERE)
https://anuragreddy72.blogspot.com/2021/05/case-discussion-on-hypokalemic-periodic.html
QUESTIONS:
1) What was the reason for coma in this patient?
The reason for coma is due to severe hypoxia, as his SpO2 levels were 20% when he was admitted. Along with this, hypokalemia leads to respiratory muscle paralysis, which may have aggravated his dyspnoea.
2) What were the competency gaps in hospital 1 Team to manage this intubated comatose patient that he had to be sent to hospital 2? Why and how did hospital 2 make a diagnosis of hypokalemic periodic paralysis? Was the coma related?
The main competency gap was in the lack of testing for serum electrolytes, as the hypokalemia had caused weakness and fatigue in this patient.
Hospital 2 make a diagnosis of hypokalemic periodic paralysis based on the fact that the patient had generalised weakness before becoming comatose, along with tingling and symptoms of paralysis. On testing serum electrolytes, his potassium levels were found to be 2.3 mEq/L (normal-3.5-5)
The coma was most probably related, as hypokalemia can cause respiratory muscle paralysis, leading to aggravation of hypoxia, hence causing unconsciousness in the patient.
3) How may covid 19 cause coma?
Yes, as the brain is extremely sensitive to oxygen, oxygen deprivation due to COVID-19 can lead to a comatose state.
This patient had very low SpO2 levels (20%), which may have caused the coma.
CASE 9-6 (COVID-19 WITH ALTERED SENSORIUM)
https://vijaykumarkasturi.blogspot.com/2021/05/65-years-old-male-with-viral-pneumonia.html
QUESTIONS:
1. What was the cause of his altered sensorium?
Probable causes include
1. Altered sensorium due to hypoxia, leading to hypercapnic encephalopthy and altered sensorium
2. Increased urea levels leading to uraemic encephalopathy, which causes altered sensorium
2. what is the cause of death in this patient?
The cause of death in this patients was due to complications of COVID-19, most probably Acute Kidney Failure (AKI), as denoted by increased urea and creatinine, and hypoproteinemia. Hypoxia and inflammatory response due to COVID-19 may have triggered the process.
Source: https://www.frontiersin.org/articles/10.3389/fphar.2020.579886/full
7) A 67 year old lady in the ICU with COVID induced Viral Pneumonia .
https://drsaranyaroshni.blogspot.com/2021/05/a-67-year-old-lady-in-icu-with-covid.html
Q1. What is the grade of pneumonia in her?
A. Based on the CT severity score it can be said that the patients pneumonia is moderate.
Q2. What is the ideal day to start steroids in a patient with mild elevated serum markers for COVID ?
A. It is best to start the treatment with dexamethasone before the onset of cytokine storm.
Q3. What all could be the factors that led to psychosis in her ?
A. The following can lead to ICU psychosis
Sensory deprivation
Sleep deprivation
Stress
Continuous light levels
Continuous monitoring
Lack of orientation
pain
drug reactions
Infections
metabolic disorders
Dehydration
Q4. In what ways shall the two drugs prescribed to her for psychosis help ?
A. Pirecetam improves memory and causes cognitive enhancement and also improves mood.
Resperidone acts by decreasing the dopaminergic and seritonergic pathways in the brain
Q5. What all are the other means to manage such a case of psychosis?
A. The management of ICU psychosis primarily depends on the cause. If it is sleep deprivation then hte patient should be provided a peaceful place to take rest.
If it is due to underlying conditions like heart failure and dehydration then these should first be corrected.
Haloperidol is a medication commonly used to manage ICU psychosis. Other common anti-psychotics can also be used.
Q6. What all should the patient and their attendants be careful about ( w.r.t. COVID )after the patient is discharged ?
A. The patient is supposed to self isolate after they are discharged for another 7 days after discharge. If possible oxygen levels are to be monitored as well for the next 7 days. The patients and the patient's attenders should be on the look out for danger symptoms such as
trouble breathing, chest pain, bluish discolouration of lips, confusion or inability to wake up.
Q7. What are the chances that this patient may go into long covid given that her "D Dimer" didn't come down during discharge?
A. Long COVID is the persistence of symptoms such as cough, breathlessnes, headaches and chest pain weeks to months after discharge. People suffering from long COVID usually have elevated biomarkers such as elevated d dimer and CRP. As this patient has elevated d dimer levels at discharge there is a good chance that she could suffer from long COVID.
8) 35YR/M WITH VIRAL PNEUMONIA SECONDARY TO COVID 19 INFECTION
https://bhavaniv.blogspot.com/2021/05/35yrm-with-viral-pneumonia-secondary-to.html?m=1
Q1. Can psoriasis be a risk factor for severe form of COVID?
A. There is no evidence that patients with moderate-to-severe psoriasis receiving systemic treatments, including biologics, have higher risk of SARS-CoV-2 infection and/or increased hospitalization and death related to COVID-19 compared to the general population.
Q2. Can the increased use of immunomodulatory therapies cause further complications in the survivors?
A. Immunomodulators help COVID 19 patients by suppressing the cytokine storm but they also have thepotentialt to increase the risk of infection (like mucormycosis), traditional clinical signs may be masked with resulting delays in identification and treatment.
Q3. Is mechanical ventilation a risk factor for worsened fibroproliferative response in COVID survivors?
A. Increasing evidence from experimental and clinical studies suggests that mechanical ventilation, which is necessary for life support in patients with acute respiratory distress syndrome as seen in COVID 19 can cause lung fibrosis, which may significantly contribute to morbidity and mortality. It is believed that ventilator induced lung injury is the cause for the fibroproliferative changes and the resultant lung fibrosis.
9) 45 year old female with viral pneumonia secondary to Covid-19
https://vidya36.blogspot.com/2021/05/comparative-study.html?m=1
Q1. What is the type of DM the patient has developed ?(is it the incidental finding of type 2 DM or virus induced type 1DM)?
A. Incedental type 2 DM can be differentiated from de novo covid induced type 1 DM with the help of the HbAc1 levels.
As HbAc1 levels are indicators of long term blood ssugar levels they are likely to be raised in pre existing DM that was incidentally discovered. But in case ofthe diabetes being de novo in nature then the HbAc1 levels are unlikely to be raised. As the patients HbAc1 levels are not raised we can not at this point determine if the patient has incedental discovered type 2 DM or Covid induced de novo DM.
Q2. Could it be steroid induced Diabetes in this patient?
A. As the patient was given dexamethasone as a part of her treatment regimen it is possible that her elevated glucose levels are a result of steroid induced hyperglycemia.
10) A little difference that altered the entire covid recovery game: a report of two patients with focus on imaging findings.
https://vidya36.blogspot.com/2021/05/comparative-study.html?m=1
Q1. What are the known factors driving early recovery in covid?
A. The following factors can lay a role:
Younger age ggroup
shorter duration of fever
No diabetes
PaO2/FiO2 levels
No comorbidities
11) Viral pneumonia secondary to COVID of a denovo Diabetes Mellitus
https://rishithareddy30.blogspot.com/2021/05/covid-case-report.html
1. How is the diabetes related to the prognosis of COVID patients? What are the factors precipitating diabetes in a patient developing both covid as well as Diabetes for the first time?
A. People suffering from diabetes are like to experience more severe symptoms of the disease than the ones who are not diabetic. Even within the patients that are diabetic the people whose disease is under better control tendtendvbe better diagnosis.
Possible causes for de nov diabetes in COVID19 include:
· The SARS CoV 2 virus enters the cells through the ACE 2 receptors which are present in large numbers in the pancreas and that this damages the pancreatic cells.
· Another theory is that the inflammation caused by the cytokine storm damages the beta cells.
Q2. Why couldn't the treating team start her on oral hypoglycemics earlier?
A. As the insulin is faster acting as compared to oral hypoglycemics and as her blood glucose level was very high it is important to bring it down as fast as possible.
12) Moderate to severe covid with prolonged hospital stay:
https://93deepanandikonda.blogspot.com/2021/05/42-years-female-patient-with-viral.html
Questions:-
1) What are the potential bio clinical markers in this patient that may have predicted the prolonged course of her illness?
Serum LDH: 571U/L (Normal range=140-280U/L
ALP : 342 U/L (Normal range=44-147U/L)
SpO2: 82% at RA (Normal range= >96%)
HR: 124bpm (Normal range=60-100bpm)
Classically, the bio clinical markers that are predictive of a Covid-19 patient's outcome are
C reactive protein [>57.9mg/dL]
D-Dimer [>1mcg/ml associated with poorer prognosis]
Serum LDH [>248U/L]
IL-6 [2.9 times higher in severe disease compared to mild disease]
SGPT [Isolated rise in SGPT >3 times the normal value]
ESR [high sustained level after recovery from infection]
Albumin
Platelet count
Neutrophil count
NLR: [>5.5]
Urea
Creatinine
High sensitivity Troponin
The patient in question has elevated levels of serum LDH and ALP. Her CRP and D-Dimer levels are not high enough to be considered as a bad prognostic factor.
Sources: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7219356/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7194951/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7896696/
13) Severe covid with first diabetes
Link to Case report log :
https://vignatha45.blogspot.com/2021/05/58-years-female-patient-with-viral.html
1) What are the consequences of uncontrolled hyperglycemia in covid patients?
Hyperglycemia can lead to anomalous glycosylation of tissue receptors throughout the body. One of these receptors happens to be ACE2, the same receptor SARS-CoV2 uses to gain entry into the host cell. In fact, glycosylation of ACE2 is necessary for the virus to establish an infection.
Uncontrolled hyperglycemia freely facilitates this glycosylation, making these patients more susceptible to Covid-19 infections and increasing the severity of the infection by helping increase the viral load (by increasing the concentration of glycosylated ACE2)
Control of blood sugar can also decrease the chances of a cytokine storm during the second phase of the infection.
Uncontrolled hyperglycemia hence, suggests a poor prognosis in Covid-19 patients.
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7188620/#:~:text=Therefore%2C%20high%20and%20aberrantly%20glycosylated,and%20a%20higher%20disease%20severity.
2) Does the significant rise in LDH suggests multiple organ failure?
Lactate dehydrogenase has 5 isoenzymes that are present in various tissues such as the heart, RBCs, lungs, liver, kidney, brain, and skeletal muscle.
Since covid-19 primarily causes lung damage, LDH3 is released into the blood giving an elevated titer.
Multi-organ damage that involves the heart (myocarditis) or kidneys (renal failure) can lead to an elevation in respected isoenzymes found in these tissues.
Hence, a significant rise in LDH indicates a poor prognosis and points towards multi-organ damage.
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7251362/
3) What is the cause of death in this case?
This patient was diagnosed with uncontrolled hyperglycemia with severe covid pneumonia.
LFT shows elevated AST, ALT, and ALP with a gross increase in bilirubin titer.
The D-Dimer is elevated (560ng/ml) and the LDH is 835U/L both of which are indicators of a poor prognosis.
The most likely cause of death in this patient seems to be ARDS.
The immediate cause of death: Most probably cardio-pulmonary arrest
Antecedent cause: Severe covid-19 pneumonia
14) Long covid with sleep deprivation and ICU psychosis
https://jahnavichatla.blogspot.com/2021/05/covid-case-discussion.html
Questions:
1)Which subtype of ICU psychosis did the patient land into according to his symptoms?
Hyperactive delirium: Manifests as agitation, restlessness, refusal to cooperate with caregivers, unprovoked mood changes, hallucinations
2)What are the risk factors in the patient that has driven this case more towards ICU psychosis?
Hypertension
History of cerebrovascular accident (makes him more prone to a new one)
Steroid use
Sedative use (Gabapentin)
COPD
3)The patient is sleep-deprived during his hospital stay. Which do you think might be the most probable condition?
A) Sleep deprivation causing ICU psychosis
B) ICU psychosis causing sleep deprivation
B) ICU psychosis causing sleep deprivation is more likely in this patient
4) What are the drivers toward current persistent hypoxia and long covid in this patient?
Elevated bio clinical markers like D-Dimer, LDH, Neutrophils, WBCs(absolute), IL-6, and CRP all contribute to persistent hypoxia and worsen the prognosis. In addition to this, ICU psychosis adds to the prolonged hospital stay.
15) Moderate Covid with comorbidity (Truncal obesity and recent hyperglycemia)
https://meghanaraomuddada.blogspot.com/2021/05/case-1-2021-42yr-old-male-with-fever.html
Questions:
1. As the patient is a non-diabetic, can the use of steroids cause a transient rise in blood glucose?
Cortisol stimulates gluconeogenesis in the liver and inhibits glycogen synthesis, increasing blood glucose. Continuous treatment with corticosteroids can lead to elevated blood glucose titers even in non-diabetics.
2. If yes, can this transient rise lead to long-term complications of New-onset diabetes mellitus?
It is still unclear if the alterations brought about by covid-19 in the glucose metabolism are permanent and persist or remit after the resolution of infection. There are ongoing studies that aim to answer these questions.
Steroid diabetes is a term coined to describe diabetes mellitus arising as a result of glucocorticoid use for more than 50 years
3. How can this adversely affect the prognosis of the patient?
Hyperglycemia in general is indicative of a poorer prognosis in a patient compared to covid patients with normal blood glucose levels.
4. How can this transient hyperglycemia be treated to avoid complications and a bad prognosis?
Oral hypoglycemics (such as sulfonylureas) are efficient at controlling blood glucose levels in non-diabetics who develop steroid-induced hyperglycemia. Most cases revert to normoglycemia after discontinuation of steroids.
5. What is thrombophlebitis fever?
Fever in response to thrombophlebitis that is caused due to release of inflammatory mediators
6. Should the infusion be stopped in order to control the infusion thrombophlebitis? What are the alternatives?
No, infusion thrombophlebitis is not grounds for discontinuation of infusions that are essential for the treatment of the case. Thrombophlebitis can be treated by local compressive dressings, NSAIDs (topical and/or systemic)
16) Mild to moderate covid with hyperglycemia
https://vaishnavimaguluri138.blogspot.com/2021/05/viral-pneumonia-secondary-to-covid-19.html
Questions:
1. What could be the possible factors implicated in elevated glycated HB ( HBA1c ) levels in a previously Non-Diabetic covid patient?
The possible factors that could have led to precipitation of diabetes in a covid-19 patient are:
Genetic susceptibility to diabetes
Pre diabetic state
Viral insult to the beta cells of the pancreas
Stress hyperglycemia due to inflammation-induced insulin resistance
High dose steroid usage
17) Covid 19 with hypertension comorbidity
https://prathyushamulukala666.blogspot.com/2021/05/a-62-year-old-male-patient-with-fever.html
1)Does hypertension have any effect to do with the severity of the covid infection.If it is, Then how?
Yes, hypertensive patients are at a higher risk of COVID 19 severity. It is already known that hypertension is assocatied with a weaker immune system and is seen in older patients which show bad prognosis when dealing with this infection. As there is a high risk of developing cardiovascular events as well as end organ failure.
2)what is the cause for pleural effusion to occur??
Pneumonia caused due to COVID-19 infection lead to increase permeability of microvascular circulation which lead to pleural effusion(exudative type)
18) Covid 19 with mild hypoalbuminemia
https://meesumabbas82.blogspot.com/2021/05/a-38-yo-male-with-viral-pneumonia.html
QUESTIONS:
1. What is the reason for hypoalbuminemia in the patient?
The reason for hypoalbuminemia in COVID_9 patient is due to increased catabolism of albumin to make amino acids as well as simulataneous decrease in albumin synthesis( albumin is a negative acute phase reactant that means its level decrease during inflammation)
2. What could be the reason for exanthem on arms? Could it be due to covid-19 infection ?
Exanthem is an eruptive skin rash seen in viral infections. Yes, this could be due to COVID-19 infection. The exanthem in COVID-19 resembles that of varicella.
2. What is the reason for Cardiomegaly?
High blood pressure might be the underlying cause for cardiomegaly in this patient.
Uncontrolled high blood pressure leads to increase in work load of the heart. To compensate this demand, the ventricles undergo remodelling leading to cardiomegaly.
3. What other differential diagnoses could be drawn if the patient tested negative for covid infection?
· Chicken pox
· Shingles
· Pytriasis
4. Why is there elevated D-Dimer in covid infection? What other conditions show D-dimer elevation?
D-dimer is increased in a COVID-19 patient. It may be related to the viral life cycle. The apoptotic processes target the endothelial cells of the vasculature resulting in triggered coagulopathy and ultimately result in increased d-dimer levels.
20) Covid 19 with first time diabetes
https://srilekha77.blogspot.com/2021/05/a-48-year-male-with-viral-pneumonia-due.html
Questions:
1)Can usage of steroids in diabetic Covid patients increases death rate because of the adverse effects of steroids???
COVID-19 infection causes systemic inflammation and cytokine storm. In order to prevent these severe conditions steroids are used.
A well-known adverse effect of steroid usage is the disruption in carbohydrate metabolism. It leads to hyperglycemia. When steroids are given to a diabetic COVID-19 patient utmost care must be taken. The patient should be shifted from oral anti diabetic drugs to s.c. insulin and blood sugars should be closely monitored. If possible, Tocilizumab should be used instead of steroids.
Steroid usage in diabetic patient has shown a increase in death rate as it further decreases the immunity of the patient and make them prone to other opportunistic infections like mucormycosis leadth to inceased death rate.
2)Why many COVID patients are dying because of stroke though blood thinners are given prophylactically?
In COVID-19 infection due to systemic inflammation and cytokine storm even when they are adequately managed, ae leading to damage of inner walls of small blood vessels of the brain. These blood vessels have very little or no collateral blood supply.
Even though the patient is on blood thinners they cannot prevent this damage. When the blood viscocity becomes higher either due to dehydration or high LDL/cholesterol levels, these small blood vessels are blocked leading to stroke.
3)Does chronic alcoholism have effect on the out come of Covid infection?If yes,how?
Yes, chronic alcoholism does worsen the prognosis of COVID-19 patient.
One of the adverse effect of chronic alcoholism is its ill effect on innate as well as adaptive immunity.
Reduced resistance to COVID-19 promotes progression of disease and leading to wrose prognosis
21) Severe Covid with Diabetes
https://sudhamshireddy.blogspot.com/2021/05/a-65-year-old-female-with-fever.html
Questions-
1. What can be the causes of early progression and aggressive disease(Covid) among diabetics when compared to non diabetics?
it is observed that there is a early as well as aggressive progression of COVID 19 in diabetics. This is attributed to interactions of several risk factors as well as hyperglycemia which is seen in diabetic patients. It modulates immune response as well as inflammatory responses thus predisposing individuals to lethal course of the disease.
2. In a patient with diabetes and steroid use what treatment regimen would improve the chances of recovery?
methylprednisolone from 40 mg/day to 160 mg/day for 6 days according to the weight and status of the patients. During this course of treatment, blood sugar should be closely monitored and patient should be shifted from oral anti diabetic drugs to insulin.
3. What effect does a history of CVA have on COVID prognosis?
It is established that COVID-19 is associated with coagulopathy. In a patient who has a history of CVA are mostly old and have other co-morbidities which leads to severe course of the disease as well as poor prognosis.
23) Covid 19 with multiple comorbidities:
https://nehae-logs.blogspot.com/2021/05/case-discussion-on-viral-pneumonia.html
1) What do you think are the factors in this patient that are contributing to his increased severity of symptoms and infection?
· Old age
· Diabetes mellitus type 2
· Chronic kidney disease
· Bronchial asthama
2) Can you explain why the D dimer levels are increasing in this patient?
It may be related to the viral life cycle. The apoptotic processes target the endothelial cells of the vasculature resulting in triggered coagulopathy and ultimately result in increased d-dimer levels
3) What were the treatment options taken up with falling oxygen saturation?
· Head elevation
· O2 supplementation
4) Can you think of an appropriate explanation as to why the patient has developed CKD, 2 years ago? (Note: Despite being on anti diabetic medication, there was no regular monitoring of blood sugar levels and hence no way to know for sure if it was being controlled or not)
During the early stage diabetes, there is a increase in blood flow to the kidneys, which strains the glomeruli and lessenstheir ability to filter blood. High levels of glucose in the blood leads to accumulation of extra material in glomeruli. It increases the stress of glomeruli inturn leading to gradual and progressive scarring. Eventually leads to the development of CKD.
10) Medical Education: (10 marks)
Experiential learning is a very important method of Medical education and while the E logs of the students in the questions above represent partly their and their patient's experiences, reflective logging of one's own experiences is a vital tool toward competency development in medical education and research. A sample answer to this last assignment around sharing your experience log of the month can be seen in the link below but while this is by a student onsite in hospital and not locked down at home we would be very interested to learn about your telemedical learning experiences from our hospital as well as community patients over the last month even while locked down at home: https://onedrive.live.com/view.aspx?resid=4EF578BAE67BA469!4180&ithint=file%2cdocx&authkey=!AOy7BpRTn42DBM
I have learnt a lot of things through online classes thank you sir.
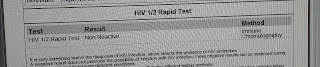
Comments
Post a Comment