A 40 y/o male with acute gastroenteritis
A 40 y/o male with complaints of loose stools and vomiting since today morning
M.sandhya
roll no 94
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box
40year old male who is a farmer by occupation and came to opd with
CHIEF COMPLAINTS;
loose stools yesterday 2 a.m
vomiting since today morning
HISTORY OF PRESENT ILLNESS;
Patient was apparently asymptomatic till yesterday evening then
he suddenly developed loose stools yesterday night @ 2 a.m 40 to 50 episodes of loose stools,large quantity, white coloured stools,foul smelling, non blood tinged
c/o vomiting 3 episodes in the morning, food particles as content,non projectile, non bilious, non foul smelling relieved on their own.for loose stools they went to local RMP and got symptomatic treatment
similar episodes of vomiting and loose stools 10 years back and got admitted for 1 week and discharged
H/O insecticides spray yesterday morning
No H/O outside food and water intake .No similar complaints to his family,neighbours
No h/o fever,cough,cold
PAST HISTORY;
N/k/c/o DM,HTN,TB,EPILEPSY, CVA,CAD,THYROID DISORDERS
FAMILY HISTORY:-
insignificant
PERSONAL HISTORY:-
DIET-mixed
APEPTITE- decreased
BOWEL &BLADDER-Increased,increased burning micturition since today
SLEEP-Adequate.
ADDICTIONS- No
GENERAL EXAMINATION:-
Patient is conscious , coherent,cooperative.
Well oriented to time place & person
Moderate built and moderately nourished.
Pallor absent
No cyanosis, clubbing, icterus, LN
Vitals :
Bp -140/100 mmhg
PR -96 bpm ;
RR : 22cpm
Spo2 : 96 on RA
GRBS:128 mg/dl
CENTRAL NERVOUS SYSTEM;
patient is conscious
speech is normal
no signs of meningeal irritation
Sensory examination: Normal
reflexes;
RIGHT LEFT
BICEPS +2 +2
TRICEPS +2 +2
SUPINATOR +1 +1
KNEE +2 +2
ANKLE +2 +2
Rhomberg's negative
Cerebellum:
Nystagmus-absent
Tremors- absent
Finger nose test- normal
Dysdiadokinesia- absent
CARDIOVASCULAR SYSTEM:-
S1 S2 heard
No murmurs.
RESPIRATORY SYSTEM:-
Dyspnea-absent
No wheeze
Breath sounds - vesicular
No Adventitious sounds
ABDOMINAL EXAMINATION:-
No tenderness
No palpable liver and spleen.
Bowel sounds - PRESENT
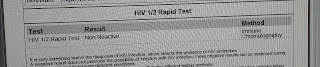
INVESTIGATIONS;
USG;
2D-ECHO;
TREATMENT ;
1.IVF 2NS.1DNS.2RL@100 ml/hr
2. Inj.metrogyl 100 ml I.V TID
3.Inj.pan 40 mg I.V OD(BEFORE breakfast)
4.Inj.zofer 10 mg I V sos
5.Inj.Neomal 1 gm I.V sos
6.Tab.dolo 650 mg PO SOS
7.Tab.Redtoil 100 mg Po/TID
8.Tab.sporolac-DS PO/TID
9.ORS in glass of water /SIPS WITH EACH EPISODES
10.Tab.OFLOX 300 mg PO/BD
11.BP.PR.RR.TEMP charting 4th hourly













Comments
Post a Comment