Internal assessment
Bone density
Bone density, or bone mineral density, is the amount of bone mineral in bone tissue. The concept is of mass of mineral per volume of bone.
It is measured by densitometry or Dexa - scan
Causes of osteoporosis;
Nutrition and Gi disorders; malnutrition, malabsorption syndromes,severe liver disesase
Endocrine; cushings syndrome, thyrotoxicosis,hyperparathyroidism, acromegaly, hypogonadism.
Rheumatological disorders; rheumatoi arthritis,ankylosong spondylosis
Inherited disorders;
Osteogenesis imperfecta,
Marfan syndrome, hemochtomatoais
Porphyria
Drugs; corticosteroid,chronic heparin therapy
Miscellaneous;immobilizaton,post menopausal,pregnancy, lactation,senile osteoporosis
Clinical features;
Fracture produces sudden pain
Common site fracture- spine ,hip,wristjoints
Vertebral fractures can occur with out pain
Lab investigations;
Serum calcium, alkaline phosphatase, urinary calcium and other relevant investigations for suspected underlying cause
* Urinary level os cross linked N- telopeptides indicate rate of bone break down or turnover
Radiograph of spine and pelvis;
Reduced cortical thickness of bones
Increased radiolucency of bones
Vertebrate shows " cod fish" appearance
Collapse of vertebral body with kyphosis
Measurement of bone density;
Quantitative CT scan
Quantitative ultrasound
Dual energy x-ray absorptiometry(DEXA) scan for bone mineral density
Treatment;
Diet should include atleast 1g of calcium and 800-1000IU of vitamin D daily.additional supplementation may be done to maintain bone and muscle strength
* Ensure adequate weight bearing exercises
*Smoking and alcohol should be stopped
Bisphosphonates;
Combined with vitD and calcium
Bisphosphonates suppress osteoclast mediated bone resorption.they accelerate osteoclast apoptosis
Risedronate :5mg orall
Alendronate10mg orall
Ibandronaye; 150mg once a month
Pamidronaye90mg iv month
A/e: git upset
Hormone replacement therapy
Recombinant human parathyroid hormone
Selective oestrogen receptor modulators; raloxifene for post menopausal osteoporosis
Salmon calcitonin
Strontium ranelage; prevention of both vertebral and non vertebral fractures
Denosumab;
Inhibits osteoclast formation ,thus decreasing bone resorption
It is a rare complication of hypothyroidism seen usually in elderly pts
More than 90% of cases occur during winter months
Causes; infections,drugs ( amiodarone, b blockers,diuretics, barbiturates,) cardiac failure, hyponatremia, hypoxia,hypercapnia
Clinical features,; depressed level of consciousness,low body temperature, bradycardia
*Neuropsychiatric manifestations.
*They develop psychosis with delusions and hallucinations (myxoedema madness) proegressed to depressed level of consciousness, convulsions,coma ( myxoedema coma).
Diagnosis;
Metabolic abnormalities; hyponatremia, hypoglycemia
Arterial blood gas ; respiratory acidosis,hypoxi,hypercapnia
Csf pressure ; low and protein content elevated
Treatment;
Supportive care;
Gentle warming with blankets,Broad spectrum antibiotics,high flow oxygen,and if required assisted ventilation
Correction of hyponatremia and hypoglycemia
Hydrocortisone (100mg ivsly,8hrly)is required due to increased metabolic stress
Thyroid hormone replacement;
T4- initially 100-150Micro gm and then 75-100 MCG iv is recommended
T4- - orally ina dose of 300mcg start followed by 100-300mcg daily
Treat precipitating causes
4)ans ; localization of spinal cord lesions
Plegia ;severe or complete weakness
Paresis : mild or moderate weakness
Monoplegia ; weakness of one limb
Paraplegia ; weakness of both lower limbs
Quadriplegia ; weakness of all 4 limbs
Diplegia ; quadriplegia in which lower limbs are affected more than upper limbs
Cord lesion above D12 segment
Acute state retention
Reflex bladder
Reflex emptying,vague sensation,small bladder
Conus lesion(
S3-CO1)
Autonomic bladder;
No bladder sensation ,dribbling, more residual urine
Cauda equina lesion (L2-co1)
Bladder sensation normal
Results of spinal cord lesion ;
At the level;
Motor; segmental LMN findings
Sensory ; segmental sensory root findings
Below the level
Motor :UMN findings
Sensory : tract involvement findings
Autonomic ; bowel.bladder
Others
Localization of C5 segment lesion
1)atC-5
a) motor LMN weakness of C5 myotome-deltoid and biceps
b) reflex; absent
c)sensory; radicular symptoms atC5
2) below C5
a) UMN findings
b) posterior column and spinothalamic tract involvement
Localization at D10 segment
Weaknesses of lower abdominal muscles
Absent lower abdominal reflex
Sensory dermatomal signs at D10
2) Below D10
a) UMN findings
b) posterior column and spinothalamic tract involvement
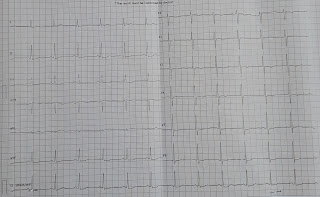
Causes; Rheumatic heart disease, ischemic heart disease, hypertension, thyrotoxicosis, congenital heart disesase, cardiomyopathy, pericardial diseases,rare causes; alcohol, pulmonary embolism
Symptoms; palpitations,fatigue,syncope,
Signs; irregularly irregular pulse
Absence of waves on jvp, hypotension,disappearance of psa of mid diastolic murmur of mitral stenosis
Disappearance of fourth heart sound
Diagnosis;
ECG; irregularly irregular rhythm of qrs complexes
Absent p waves
Small irregular waves at state of 350-600/minute
Complications ; syncope,angina, thromboembolism
Hypotension.
Management;
Goals;
Hemodynamic stabilization
Control of ventricular rate
Restoration of sinus rhythm
Treatment of underlying cause
1) if pt s clinical status is severely compromised synchronised dc cardioversion is treatment of choice
2) if pts cardioversion is not severely compromised treatment is in 2steps
*Slowing ventricular rate with diltiazem,verapamil,digoxin
Amiodarone; 150mg over 10 minutes followed by 1mg / minute over 6hrs and0.5mg/minute for another 18hrs
A/E; hepatic toxicity, pulmonary toxicity, thyroid dysfunction
2(converting rhythm to normal sinus rhythm
Pharmacological cardioversion to sinus rhythm with quinidine,flecanide
*Antithrombotic therapy
*Aspirin
*Refractory cases are managed with catheter ablation therapy
* Abnormal erythroblasts seen in bone marrow of pts with deficiency of vitamin B12,folate orboth
Megaloblasts abnormally large in size and nucleated,well hemoglobinized
* Macrocytes are erythrocytes with increased mcv
Causes: vitaminb12 or folate deficiency, liver disease,alcohol,aplastic anemia, Hypothyroidism, sideroblastic anemia,nitrous oxide abuse
Peripheral smear;
Macroovalocytes and hypersegmented neutrophils ,poikilocytosis,fragmented rbcs
Investigations; HB-reduced
MCV; raised>120fl
RBC count; reduced
Reticulocyte count: reduced
TLC; reduced
Platelet count : reduced
Indirect bilirubin mildly elevated
Serum iron elevated
Tibc reduced
Serum ferritin increased
Plasma LDH markedely increased
Bone marrow;
Hypercellular, megaloblatic erythroid cells, giant megakaryocytes,dysplastic megakaryocytes, marrow iron stores increased
Specific tests; reduced serumb12or folate
Management;
Supportive therapy;
* Blood transfusion s
* Treatment of infections
* Treatment of cardiac failure
Specific therapy
* Treatment of underlying cause vit B12 or folate deficiency
*VitaminB12 therapy
*Folate therapy
causes of ascites
Hepatic cirrhosis,
*Malignant; hepatic, peritoneal
*Infection; tuberculosis,bacterial peritonitis
*Hypoproteinemia; Nephrotic syndrome, malnutrition
*Cardiac failure, constrictive pericarditis
*Hepatic venous obstruction; budd-chiari syndrome,veno occlusive disease
*Pancreatitis
*Lymphatic obstruction-chylous ascites
In common; meigs syndrome, vasculitis, Hypothyroidism,
Pathogenesis;
Ascites occurs due to imbalance between formation and resorption of peritoneal fluid.in cirrhosis of liver ascites is due to
* Portal hypertension
*Renal changes; increased sodium and water resorption.thre is stimulation of RAAS,increased ADH release and decreased release of natriuretic hormone or third factor
*Imbalance between formation and removal of hepatic and gut lymph
*Hypoalbunemia
*Elevated Padma vasopressin and epinephrine levels in response to volume depleted state accenuates renal and vascular factors
Differential diagnosis;
Acute liver failure,cirrhosis, budd-chiari syndrome,dilated cardiomyopathy, alcoholic hepatitis, biliary disease
approach to Acute pancreatitis
* Inflammation of pancreas.
Etiology; alcoholic ingestion,biliary calculus
Post ercpa,trauma to abdomen
*Metabolic : renal failure,hypercalcaemia,hypertryglyceridemia
*Penetrating peptic ulcer
* Connective tissue disorders; systemic lupus erythematosus,polyarteritisnodosa
* Infections; viral hepatitis,mumps
* Drugs: sulphonides, tetracycline s,
Hereditary
Pathology;
Oedematous pancreatitis; diffuse enlargement of pancreas with lack of pancreatic parenchymal necrosis
Necrotsing pancreatitis
*Hemorrhagic pancreatitis
Clinical features;
Symptoms;
* Cardinal symptom of acute pancreatitis is;
Pain- mild to severe intensity,dull and boring and steady,sudden pain in onset and gradually increase es in severity
Located in epigastric region,though may be percieved more on left or right side depending on which portion of pancreas is involved
Radiates directly through abdomen to back
Partial relief if sits up and leans forward s
Lasts more than 1 day
*Nausea and vomiting
*Anorexia
Signs;
*Fever low grade
Tachycardia
Tachypnoea
Hypotension,jaundice, abdominal tenderness,muscle guarding,and distension,bowel sounds - hypoactive
Lungs; cyanosis,basal crepitation s, pleural effusion
Skin;
Cullen sign; bluish discoloration around umbilicus
Grey Turner sign; bluish discoloration in flanks due to hemoperitoneum
Others : hematmesis,melena
Investigations;
Serum amylase; initial increase in 24hours and then decline to normal in2-3 days
Serum lipase; preferable for diagnosis
Takes longer time to clear from blood
*Marked elevation in pleural or peritoneal fluid(>5000IU/dl)suggests pancreatitis
Other; blood glucose,total leucocyte count, platelet count,blood urea,serum creatinine,and other electrolytes, triglycerides,
Blood gas
Plain x-ray abdomen and chest
Ultrasound of abdomen
Ct scan of abdomen; show solid mass of swollen pancreas (phlegmon),pseudocyst or pancreatic abscess
Mri abdomen;
Endoscopic ultrasound
Treatment;
Nil oral initially with gradual return to oral intake as abdominal pain recedes and hunger return s.enteral feeding should be restarted in severe cases .this can be done by oral intake or useof nasogastric tube
* Iv fluids to maintain intravascular volume in first few days
* Analgesics for pain relief
*Nasogastric aspiration if pain continues
*Monitor pulse,bp, abdomen girth, urine output,blood glucose, calcium, blood gases
*Prophylactic antibiotics; ,carbepenams(imepenam,meropenam),ceftazidimein severe cases
*Other drugs; ppis, glucagon,octreotide and aprotinin
* Surgery ;
Infected pancreatic necrosis
Complications
ERCP with in first 36-48hours in pts with gallstones pancreatitis
Complications;
Local;
Necrosis
Pseudocyst,pancreatic abscess, pancreatic ascites, obstructive jaundice
Systemic;
Hypovolemic shock,ARDS,renal failure,fat necrosis,pleural effusion,DIC,muliple organ failure.
*Weakness; voluntary movements are disturbed; distal predominant
Tone; hypertonia( claspknife spasticity)
*Reflex (superficial); absent or decreased
*Reaction of degeneration; absent
Weakness; paralysis of muscles supplied by that segment or nerve proximalpredominant
*Reflex (tendon); decreased or absent
*Reflex (superficial); absent or decreased
Plantar response; flexor or absent
*Fasciculations ; often present
*Bilateral movements; affected
✓Acute renal failure
✓Toxins
✓Drugs
✓Chronic renal failure patients awaiting renal transplantation
✓patients with CRF in whom quality of life has deteriorated
renal manifestations of snake bite
✓ Hematuria
✓Hemoglobinuria
✓Myoglobinuria
✓Loin pain
✓Renal failure
13Q). Causes of portal hypertension
13] ans; causes of portal hypertension
✓ Heart; constrictive pericarditis
✓inferior vene cava; congenital webs,tumor invasion, thrombosis
✓large hepatic veins; thrombosis,webs, tumor invasion
✓Small hepatic veins; veno occlusive disease
✓portal vein: thrombosis
✓splenic vein; thrombosis, invasion or compression by tumors
✓post sinusoidal causes; veno occlusive disease, alcoholic hyaline sclerosis
✓ sinusoidal causes ; cirrhosis,acute alcoholic hepatitis. Cytotoxic drugs,vitamin A intoxication
✓pre sinusoidal causes; schistosomiasis,non cirrhotic portal fibrosis, sarcoidosis,toxins, idiopathic
14)Q. Clinical features of Downs syndrome





















Comments
Post a Comment