M.sandhya rollno;89 9th semester
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
CASE DISCUSSION:
A 28 year old male farmer by occupation came to the opd with the chief complaints of fever since 15 days and shortness of breath since 3 days
History of present illness :
This patient is farmer by occupation wakes up at 5 o clock every day and goes for his work and used to have breakfast (rice and curry) around at 8am and at 1 pm he had mixed type of diet which includes rice and dal more frequently and comes back his home at around 6pm and he usually used to have dinner at 8pm and he goes to his bed at around 9pm
he is occasional alcoholic
15 days back he had fever which is insidious in onset associated with chills and rigours for that he was taken to local hospital and they gave medications but fever was not subsided and he brought up to our hospital on 20/10/21 for further evaluation
patient was apparently asymptomatic 15 days back then he had fever which is insidious in onset gradual in progression high grade continuous not relieved on medication and associated with chills and rigour
he also had shortness of breath which is sudden in onset progressing from grade 2 to 3aggravated on walking ,taking rest no relieving factors
no history of loose stools and pedal edema
no history of bleeding manifestations, bleeding gums,malena,haemoptysis and haematemesis
past history:
Not a k/c/o DM, HTN , TB ,Asthama ,CVA/CAD , EPILEPSY and thyroid
no significant surgical history
no transfusion of blood
personal history:
Diet: mixed
Appetite decreased
Sleep inadequate
patient had constipation normal bladder filling and micturition
drinks occasionally
GENERAL EXAMINATION:
Patient is conscious, coherent and cooperative
Moderately built and moderately nourished & dehydrated
No pallor,icterus,clubbing,cyanosis,koilonychia,edema and lymphadenopathy
VITALS:
Temp: 100.6F
PR: 72;bpm
BP:80/60 mm hg
RR: 16cpm
Spo2 - 98% at RA
SYSTEMIC EXAMINATION :
CVS:
Inspection:
Chest wall is bilaterally symmetrical.
No precordial bulge
No visible pulsations, engorged veins, scars, sinuses
palpation:
JVP: normal
Apex beat: felt in the left 5th intercostal space in the mid clavicular line.
Auscultation:
S1, S2 heard , No murmurs
RESPIRATORY SYSTEM:Position of trachea: central
Bilateral air entry +
Normal vesicular breath sounds - heard
No added sounds.
PER ABDOMEN:
Abdomen is soft and tenderness present in the epigastric region .
No organomegaly.
Bowel sounds heard.
No palpable mass or free fluid
CNS :
Patient is Conscious
Speech: normal
No signs of Meningeal irritation
Motor & sensory system: normal
Reflexes: present
Cranial nerves: intact
PROVISIONAL DIAGNOSIS:viral pyrexia under evaluation.
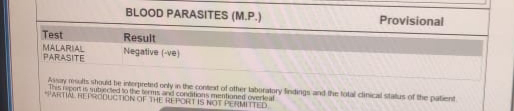
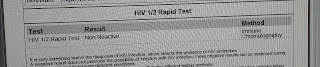
INVESTIGATIONS:
Hemogram(20/10/21)
on 22/10/21
SERUM ELECTROLITE (20/10/21)
BLOOD UREA (20/10/21)
SERUM CREATININE (20/10/21)
RAPID DENGUE TEST
SEROLOGY ;NEGATIVE
CHEST X RAY
ECG
TREATMENT
DAY 1
1)IV Fluids NS and RL -100 ml/hr
2)inj optineurin 1 amp in 100 ml/hr IV bd
3)inj Monocef 1gm IV bd
4)Tab.Doxycyline 100 mg po bd
5)inj pan 40 mg IV od BBF
6)inj zofer 4 mg IV SoS
7) inj Neomol 1 gm iv SoS
8)Tab .Dolo 650 mg po sos
9 ) Bp temp,PR monitoring 6 th hourly ,inform SOS
DAY 2
1)IV Fluids NS and RL -100 ml/hr
2)inj optineurin 1 amp in 100 ml/hr IV bd
3)inj Monocef 1gm IV bd
4)Tab.Doxycyline 100 mg po bd
5)inj pan 40 mg IV od BBF
6)inj zofer 4 mg IV SoS
7) inj Neomol 1 gm iv SoS
8)Tab .Dolo 650 mg po sos
9 ) Bp temp,PR m
SOAP NOTES
DAY 1
AMC bed 2
21/10/21
S: fever present
O: pt is conscious coherent and cooperative
O/E
PR: 72 BPM
BP: 80/60 mmHg
RR :18 Cpm
Temp:98.6F
CVS: S1,S2 heard
RS NVBS +
P/A
Soft non tender
Bowel sounds+
CNS : NFD
A:viral pyrexia under evaluation
P:
1)IV Fluids NS and RL -100 ml/hr
2)inj optineurin 1 amp in 100 ml/hr IV bd
3)inj Monocef 1gm IV bd
4)Tab.Doxycyline 100 mg po bd
5)inj pan 40 mg IV od BBF
6)inj zofer 4 mg IV SoS
7) inj Neomol 1 gm iv SoS
8)Tab .Dolo 650 mg po sos
9 ) Bp temp,PR monitoring 6 th hourly ,inform SOS
DAY 2
AMC bed 2
22/10/21
S: no present complaints
O: pt is conscious coherent and cooperative
O/E
PR: 66 BPM
BP: 90/60 mmHg
RR :18 Cpm
Temp:98.6F
CVS: S1,S2 heard
RS NVBS +
P/A
Soft non tender
Bowel sounds+
CNS : NFD
A:viral pyrexia under evaluation
P:
1)IV Fluids NS and RL -100 ml/hr
2)inj optineurin 1 amp in 100 ml/hr IV bd
3)inj Monocef 1gm IV bd
4)Tab.Doxycyline 100 mg po bd
5)inj pan 40 mg IV od BBF
6)inj zofer 4 mg IV SoS
7) inj Neomol 1 gm iv SoS
8)Tab .Dolo 650 mg po sos
9 ) Bp temp,PR monitoring 6 th hourly ,inform SOS















Comments
Post a Comment