52 year old male with fever,tightness of abdomen and decreased appetite
52 Year old male with fever and tightness of abdomen
RESPIRATORY SYSTEM:
INVESTIGATIONS
M.sandhya
1701006117
june8th,2022
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box
52 year old male resident of nalgonda farmer by occupation and came to opd with the
CHIEF COMPLAINTS;
fever since 4 days
tightness of abdomen since 3 days
decreased appetite since 2 days
HISTORY OF PRESENT ILLNESS
patient was apparently asymptomatic 4 days back then he had fever which is insidious in onset low grade continuous fever gradual in progression not associated with chills and rigors no aggravating factors relieved with medications and he had tightness of abdomen which is sudden in onset and non progressive associated with breathlessness which is of grade 4, and pain which is squeezing type and non radiating not associated with pedal oedema vomiting diarrhoea
he also had decreased appetite
no h/o melaena,diarrhoea hematemesis,nausea,loss of weight, orthopnea
HISTORY OF PAST ILLNESS
no similar complaints in the past
not a k/c/o DM,HTN,ASTHMA,THYROID
CVA/CVD
NO significant surgical history
no h/o blood transfusion
FAMILY HISTORY
insignificant
PERSONAL HISTORY
Diet;mixed
appetite; decreased
sleep; adequate
bowel and bladde; regular
addictions; toddy (occasionally)
no drug allergy
GENERAL EXAMINATION
Patient is conscious, coherent,cooperative.
Well oriented to time place & person
Moderate built and moderately nourished
no pallor,icterus,cyanosis,clubbing, lymphadenopathy
VITALS
pulse rate; 82 bpm
respiratory rate; 18 cpm
blood pressure; 120/80
temperature: afebrile
spo2; 99
GRBS;106
SYSTEMIC EXAMINATION :
CVS:
Inspection:
Chest wall is bilaterally symmetrical.
No precordial bulge
No visible pulsations, engorged veins, scars, sinuses
palpation:
JVP: normal
Apex beat: felt in the left 5th intercostal space in the mid clavicular line.
Auscultation:
S1, S2 heard , No murmurs
Position of trachea: central
Bilateral air entry +
Normal vesicular breath sounds - heard
No added sounds.
PER ABDOMEN:
Abdomen is soft and tenderness present in the epigastric region .
mild spleenomegaly seen
Bowel sounds heard.
No palpable mass or free fluid
CNS :
Patient is Conscious
Speech: normal
No signs of Meningeal irritation
Motor & sensory system: normal
Reflexes: present
Cranial nerves: intact
PROVISIONAL DIAGNOSIS;viral pyrexia with throbocytopenia and with mild ascites
CLINICAL IMAGES;
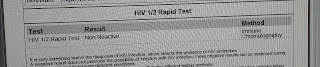
INVESTIGATIONS
haemoram;
Blood urea;
Serum electrolytes;
Serum creatinine;
TREATMENT
I.v fluids -NS,RL 100 ml /hour
inj.pan 40mg I.v/OD
inj .optineuron 1 amp
inj.zofer 4mg I.V











Comments
Post a Comment