A 73 y/o female with SOB and chest pain since 2 days
73 year old female with SOB and CHEST PAIN since 2 days
M.sandhya
march 3rd,2023
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box
73 year old female who is a home maker and came to opd with
CHIEF COMPLAINTS;
shortness of breath and chest pain since 2 days
HISTORY OF PRESENT ILLNESS;
Patient was apparently asymptomatic 15 years back and gradually developed weakness (generalized) and went to hospital and diagnosed with type 2 DM and HTN and was prescribed medication.she was fine till 15 days back and then she developed fever with generalized weakness and went to hospital and diagnosed to have ?chronic kidney disease with base line creatinine 2.9
PAST HISTORY
k/c/o HTN since 15 years and on regular medication
k/c/o,DM type 2 since 15 years and was on OHAS
for 7 years and then later shifted to insulin.
presently on inj.MIXTARD,25 U (M) and 20 U(night)
FAMILY HISTORY:-
insignificant
PERSONAL HISTORY:-
DIET-mixed
APEPTITE- decreased
BOWEL &BLADDER-Regular
SLEEP; adequate
GENERAL EXAMINATION:-
Patient is conscious , coherent,cooperative.
Well oriented to time place & person
Moderate built and moderately nourished.
Pallor present
No cyanosis, clubbing, icterus, LN
B/L pedal edema present
Vitals :
Bp -170/100mmhg
PR -110 bpm ;
RR : 22cpm
Spo2 : 94 on RA
GRBS:339mg/dl
CNS examination:
SYSTEMIC EXAMINATION :
CENTRAL NERVOUS SYSTEM;
CNS: R L
Tone- UL N N
LL N N
Power-UL 4/5 4/5
LL 4/5 4/5
Reflexes- Biceps- + +
Triceps- + +
Supinator- + +
Knee- + +
Ankle- + +
Plantar- flexion flexion
Sensory examination: Normal
Rhomberg's negative
Cerebellum:
Nystagmus-absent
Tremors- absent
Finger nose test- normal
Dysdiadokinesia -absent
CARDIOVASCULAR SYSTEM:
S1 S2 heard
No murmurs.
RESPIRATORY SYSTEM:-
Dyspnea- No
No wheeze
Breath sounds - vesicular
No Adventitious sounds
ABDOMINAL EXAMINATION:-
No tenderness
No palpable liver and spleen.
Bowel sounds - present.
INVESTIGATIONS:-
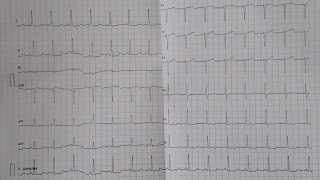
ECG;
CHEST X-RAY
2D-ECHO
USG ABDOMEN:
TREATMENT;
1. Inj.lasix 40 mg I.v/BD if SBP greater than 110 mmgh
2.T.shelcal 500 mg po/OD
3.T.nodosis 500 mg po/OD
4.T.orofer XT PO/OD
5.T.cinod 10 mg po/OD
6.T.Met-XL 12.5 mg PO/OD
7.inj.Human actrapid insulin s/c TID acc to sliding rule
8.GRBS charting
9.T.Ecosprin Av 75/10 PO/HS
10.I/O charting












Comments
Post a Comment